Clinical Research
(CR-012 (GR-004)) Dehydrated Human Amnion Chorion Membrane (DHACM) Use in Patients with Emergent Craniectomies Demonstrates Minimal Dural Adhesions at Time of Cranioplasty
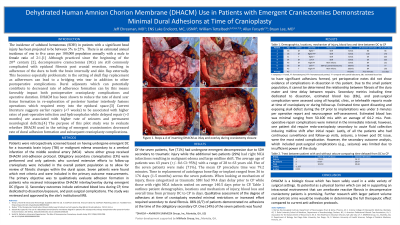
Decompressive craniectomies (DCs) are commonly complicated with epidural fibrosis post cranial resection, resulting in adherence of the dura to both the brain internally and skin flap externally. The purpose of this case series was to evaluate whether DHACM used in the setting of emergent craniectomies decreased dural adhesion formation, operative re-exposure time, and subsequent cranioplasty complications. Using mixed methods, researchers re-examined patients who underwent emergent DC with DHACM use for adhesion formation, estimated blood loss, time dedicated to dissection/exposure, and post-surgical complications upon subsequent delayed cranioplasties (CPs) (N=7). The inclusion criteria for DC included traumatic brain injury (TBI) or malignant edema secondary to a cerebral infarction of the middle cerebral artery (MCA). At the time of DC patients received DHACM anti-adhesion protocol. Qualitative data on adhesion formation in patients who received intraoperative DHACM interlay/overlay during emergent DC are summarized. Secondary outcomes including estimated blood loss during CP, time dedicated to dissection/exposure, and post-surgical complications are reported using descriptive statistics. The study was reviewed and approved by the site's institutional IRB. Of the seven patients, five (71%) had undergone emergent decompression due to SDH secondary to TBI while the additional two patients (29%) had right MCA infarctions resulting in malignant edema and large midline shift. Qualitative assessment determined 86% (6/7) of patients demonstrated no adhesions at the time of the CP. One patient (14%) was found to have significant adhesions formed, yet perioperative notes did not show evidence of complications in dissection in this patient. Secondary metrics revealed the estimated time spent dissecting and exposing skull defect prior to implantations was under 3 minutes and the estimated blood loss was minimal ranging from 50-100 mLs with an average of 64.2 mLs. Lastly, of all the patients who had continuous surveillance and follow-up visits, seizures, a known post DC issue, were the most noted complication. However, the secondary outcome analysis, which included post-surgical complications (e.g., seizures) was limited due to insufficient power of the study.
Methods:
Results:
Discussion:
DHACM’s potential as a physical barrier which can aid in supporting an intracranial environment capable of ameliorating reactive fibrosis in decompressive craniectomy patients is promising. Further research with larger patient population and controls arms would be invaluable in determining the full therapeutic effect compared to current anti-adhesion protocols.
Trademarked Items: DHACM = AMNIOFIX (MIMEDX Group, Inc, Marietta, GA, US)
References: 1. Tenny S, Thorell W. Intracranial Hemorrhage. [Updated 2023 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470242/
2. Kocher T. Die therapie des hirndruckes Hirnerschütterung. Hirndruck und chirurgische Eingriffe bei Hirnkrankheiten. 1901;3:262–6.
3. Subach BR, Copay AG. The use of a dehydrated amnion/chorion membrane allograft in patients who subsequently undergo reexploration after posterior lumbar instrumentation. Adv Orthop. 2015;2015:501202. doi:10.1155/2015/501202
4. Smith M. Refractory Intracranial Hypertension: The Role of Decompressive Craniectomy. Anesth Analg. 2017;125(6):1999-2008. doi:10.1213/ANE.0000000000002399

.png)
