Practice Innovations
(PI-024) Decreasing nursing workload: Simplifying wound management with an innovative transforming powder dressing
Introduction
The current nursing shortage is expected to intensify, especially as an aging population continues to burden healthcare systems1. Nursing shortages directly impact the patient care pathway. Lack of sufficient caregiver resources negatively affect proper wound management and treatment and increase both time to wound healing and overall hospital length of stay (LOS).2,3 We investigated if simplifying wound management by utilizing an extended wear transforming powder dressing (TPD), instead of current standard of care (SOC), would decrease nursing workload by reducing requisite dressing changes and time associated with wound care, without compromising overall outcomes.
Methods:
Methods
TPD is a commercially available dressing comprised primarily of hydrogel polymers like those used in contact lenses. When hydrated with saline, TPD aggregates to form a moist, oxygen-permeable barrier that covers and protects the wound while releasing excess exudate through vapor transpiration. TPD may be left in on the wound for up to 30 days and topped off as needed without requiring primary dressing changes.
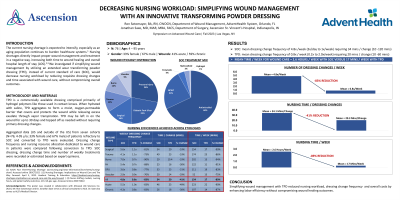
Aggregated data (US and OUS) from seven cohorts (N=76; 4-95 y/o; 33% female and 67% male) of patients refractory to SOC and converted to TPD were evaluated. Dressing change frequency and nursing resource allocation dedicated to wound care in patients were compared following conversion to TPD. SOC dressing, dressing change time and number of weekly treatments were recorded or estimated based on expert opinions.
Results:
Results
Acute (41%) and chronic (59%) wounds with traumatic (13%), surgical (16%), burn (12%), pressure injury (28%), diabetic foot ulcer (22%) and vascular (9%) etiologies were assessed. SOC treatment included antimicrobial, enzymatic, hydrogel and hydrocolloid dressings, as well as negative pressure wound therapy. SOC dressing change frequency ranged from 3x/day to 1x/week (mean=4.8) requiring 10 to 120 minutes/change (mean=34).
Mean dressing change frequency and required times were 83% and 41% lower, respectively, in patients treated with TPD compared to SOC, ranging from 0.2 to 2x/week (mean=0.8) and 10 to 60 minutes/change (mean=20). All wounds healed without complications. Pain reduced in patients with reported pain.
Discussion:
Discussion
Simplifying wound management with TPD reduced nursing workload, dressing change frequency and overall costs by enhancing labor efficiency without compromising wound healing outcomes.
Trademarked Items: Altrazeal TPD
References:
References:
1. AACN Fact Sheet-Nursing Shortage Aacnnursing.org/news-information/fact-sheets/nursing-shortage. Accessed online 28OCT2022.
2. Nursing Shortages: Implications on Wound Care and The Way Forward. April 5, 2022. Healiant Training & Education. https://healiant.com/nursing-shortages-implications-on-wound-care-and-the-way-forward/ Accessed online 29OCT2022.
3. Nurse staffing models, nursing hours, and patient safety outcomes. Nlm.nih.gov.

.png)