Health Economics
(HE-003) Comparative Effectiveness Analyses With and Without Advanced Skin Substitute Products for Medicare Beneficiaries With Diabetic Foot Ulcers (DFU’S)
Methods:
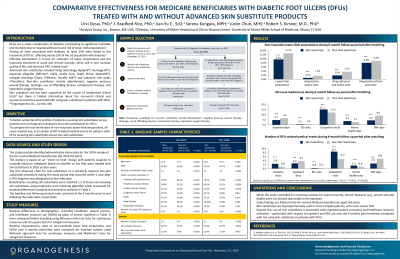
The 100% Medicare Fee-For-Service data in Standard Analytic File (Q1 2015-Q4 2021) were used to identify two mutually-exclusive cohorts of beneficiaries with DFUs: (i) beneficiaries who received skin substitutes* (index date: first claim), and (ii) beneficiaries who received conventional or advanced wound care but not skin substitutes* (index date: random). Beneficiaries were required to have continuous enrollment in Medicare Parts A and B >6 months before and after the index date. Beneficiaries receiving skin substitutes* were matched 1:1 to those not receiving skin substitutes* using propensity score matching. Outcomes over 6 months post-index were compared between matched cohorts using statistical tests for paired data. P-values < 0.05 were considered statistically significant and standardized differences (SD) >10% were considered large.
Results:
Among beneficiaries meeting the selection criteria, 59,269 received skin substitutes* and 527,799 did not receive skin substitutes*. Compared to beneficiaries not receiving skin substitutes*, those receving skin substitutes* had greater disease severity before treatment initiation, indicated by longer duration of active ulceration (5.5 vs. 3.4 months), higher rates of DFU-related infections (68.2% vs. 47.4%), non-traumatic lower-limb amputations (12.6% vs. 6.4%), and higher total medical costs ($35,007.5 vs. $23,005.7). During 6-month follow-up period, matched beneficiaries receiving skin substitutes* (N=58,491) had lower rates of non-traumatic lower-limb amputations (9.7% vs. 12.7%; SD =9.34%; p < 0.001). Additionally, beneficiaries receiving skin substitutes* had shorter stays (4.7 vs. 6.6 days), lower costs for hospitalization ($10,388 vs. $13,891) and skilled nursing facility (4.4 vs. 9.0 days; $1,887 vs. $3,435) than similar beneficiaries not receiving skin substitutes* (SD >10% and p < 0.001 for all comparisons).
Discussion: The study suggests that skin substitutes* are disproportionately used to treat or manage more complex beneficiaries, with more severe DFUs. After adjusting for baseline differences, beneficiaries receiving skin substitutes* had lower rates of amputations, lower costs for hospitalization and skilled nursing facility visits than those not receiving skin substitutes*.
Trademarked Items:
References: NOTE: * ”Skin substitutes” is a Medicare classification term for a class of celular and tissue-based products, but does not accurately describe the product’s clinical function. Skin substitutes included living technology (Apligraf, Dermagraft), placental allografts (Affinity, Epifix, Grafix Core, Grafix Prime, Nushield), collagen dressings (Oasis, PriMatrix, PuraPly AM) and cadaveric skin grafts (TheraSkin)
DISCLOSURE: Funding provided by Organogenesis. Data analysis performed by Analysis Group.

.png)
