Case Series/Study
(CS-122) Using a polylactic acid matrix for achieving wound healing in challenging wounds
Chronic wounds are characterized by being arrested in the inflammatory phase of healing. This disruption of the healing cascade leads to wound beds that have a high content of inflammatory cells and mediators, poor vascularization, and a low healing potential. Polylactic acid (PLA) matrices have shown initial success in promoting the shift from inflammation into proliferation. Here, we show our experience in using this technology in a cohort of patients with challenging chronic wounds.
Methods:
A series of 12 patients with chronic wounds, including diabetic foot ulcers, venous ulcers, and inflammatory ulcers, received weekly applications of PLA matrices until healing. The application protocol consists of “preparing the wound for healing,” which includes a thorough debridement of non-viable tissue, tissue preservation wherever possible, and optimization of comorbidities and nutritional status, followed by the application of PLA matrices under a non-adherent dressing. Secondary absorbent dressings were used and changed as often as needed. Digital planimetry was used to measure wound size and assess its change over time.
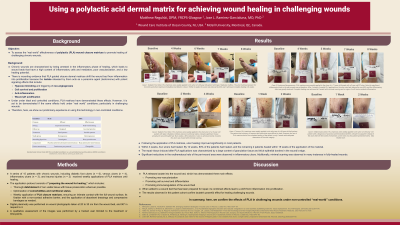
Results:
Following the application of PLA matrices, ulcer healing improved significantly in most patients. Within 3 weeks, four ulcers had healed. By 12 weeks, 80% of the patients had healed, and the remaining 2 patients healed within 15 weeks of the application of the material. The repair tissue induced after PLA applications were characterized by a significant content of granulation tissue and thick epithelial borders in the wound’s edge. Significant reductions in the erythematous halo of the peri-wound area were observed in inflammatory ulcers. Additionally, minimal scarring was observed in many instances in fully-healed wounds.
Discussion: PLA releases lactate into the wound bed, which has demonstrated three main effects: promoting neo-vascularization, promoting cell survival and differentiation, and promoting immunoregulation of the wound bed. When added to a wound bed that has been prepared for repair, its combined effects lead to a shift from inflammation into proliferation. The results observed in this patient cohort confirm lactate's powerful effect for healing challenging wounds.
Trademarked Items: SupraSDRM
References: 1. Mirhaj M, Labbaf S, Tavakoli M, Seifalian AM. Emerging treatment strategies in wound care. Int Wound J. 2022 Nov;19(7):1934–54.
2. Ring A, Goertz O, Al-Benna S, Ottomann C, Langer S, Steinstraesser L, et al. Accelerated angiogenic induction and vascular integration in a novel synthetic scaffolding matrix for tissue replacement. Int J Artif Organs. 2010 Dec;33(12):877–84.
3. Haller HL, Sander F, Popp D, Rapp M, Hartmann B, Demircan M, et al. Oxygen, pH, Lactate, and Metabolism—How Old Knowledge and New Insights Might Be Combined for New Wound Treatment. Medicina. 2021 Nov;57(11):1190.

.png)