Case Series/Study
(CS-118) Using a polylactic acid matrix for achieving wound epithelization in patients with pyoderma gangrenosum
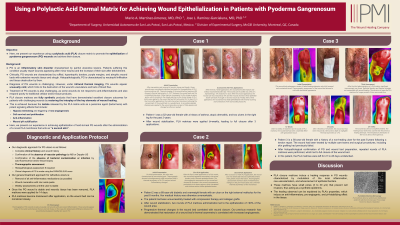
Pyoderma gangrenosum (PG) is characterized by hard-to-heal wounds refractive to most common treatments. Here, we present our experience using a polylactic acid (PLA) closure matrix to promote the epithelization of PG wounds and achieve their closure.
Methods:
Patients with shallow PG wounds received PLA matrices designed to be used “as a second skin.” After confirming a lack of bacterial contamination by fluorescence imaging, the matrices were applied and left undisturbed for 14 days. PLA matrices have been demonstrated to enhance epithelial cell migration, promote neo-vascularization, and modulate the inflammatory and acid-base environments, thus leading to improved healing.
Results:
For refractive ulcers, the general treatment algorithm for PG wounds in our centre includes removal from all anti-inflammatory medications whenever possible, confirmation of the absence of bacterial contamination through fluorescence imaging, monitoring of the inflammatory environment through thermal imaging, and daily applications of zinc oxide paste until the wound is macerated and the necrotic tissue removed. Patient 1 had two PG ulcers on the left leg for over 2 years. Once a clean wound bed was achieved, PLA matrices were applied over the ulcers for 14 days, leading to a thin epithelial layer over the wound. A second application of the matrices was prescribed, leading to the full closure of both wounds 14 days later. Patient 2 had a PG wound on the dorsum of the left foot. Despite extensive treatment, the wound proved very difficult to heal and had extensive scarring tissue around it. However, after 3 rounds of applying PLA matrices for 14 days, significant wound closure was achieved. The resulting epithelial tissue was more supple and thinner than the surrounding tissue, where no matrices were used. Patient 3 had a PG ulcer on the right leg for 9 months. After just one round of PLA matrix application, the wound was fully closed. Thermal imaging of the wound bed demonstrated a significant increase in the temperature of the wound area, which is highly suggestive of improved perfusion to its bed.
Discussion:
The use of PLA matrices as a skin barrier in PG wounds that have been cleaned and prepared for treatment is associated with their robust epithelization. This effect can be explained by PLA’s properties, which induce an anti-inflammatory, pro-angiogenic, and pH-stabilizing effect in the tissue. In the context of PG, this helps stabilize the wound’s environment and promote ulcer healing.
Trademarked Items: Suprathel CW
References: 1. Delaleu J, Lepelletier C, Calugareanu A, De Masson A, Charvet E, Petit A, et al. Neutrophilic dermatoses. Rev Med Interne. 2022 Dec;43(12):727–38.
2. Maronese CA, Pimentel MA, Li MM, Genovese G, Ortega-Loayza AG, Marzano AV. Pyoderma Gangrenosum: An Updated Literature Review on Established and Emerging Pharmacological Treatments. Am J Clin Dermatol. 2022 Sep;23(5):615–34.
3. Ring A, Goertz O, Al-Benna S, Ottomann C, Langer S, Steinstraesser L, et al. Accelerated angiogenic induction and vascular integration in a novel synthetic scaffolding matrix for tissue replacement. Int J Artif Organs. 2010 Dec;33(12):877–84.
4. Haller HL, Sander F, Popp D, Rapp M, Hartmann B, Demircan M, et al. Oxygen, pH, Lactate, and Metabolism—How Old Knowledge and New Insights Might Be Combined for New Wound Treatment. Medicina. 2021 Nov;57(11):1190

.png)