Case Series/Study
(CS-117) Using a novel polylactic acid matrix for achieving closure and limb salvage in hard-to-heal wounds
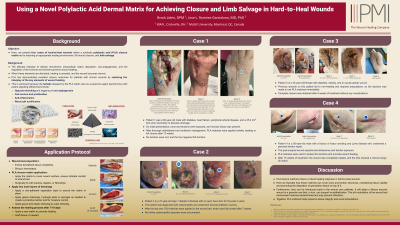
The interplay of cellular recruitment, extracellular matrix deposition, neoangiogenesis, and the immune environment governs wound healing. When these elements are disturbed, healing is arrested and the wound becomes chronic. Here, we present four cases of hard-to-heal wounds where a synthetic polylactic acid (PLA) closure matrix led to restoring an appropriate healing environment, full wound closure, and limb salvage.
Methods:
Patients with hard-to-heal wounds received weekly applications of PLA matrices. These scaffolds enhance cellular growth, promote neo-vascularization, and modulate the inflammatory and acid-base environments, thus leading to improved healing.
Results:
Patient 1 was a 60-year-old male with diabetes, heart failure, peripheral arterial disease, and a 25.2 cm2 infected foot ulcer. On initial presentation, bone and tendons were exposed, and necrotic tissue was present. After debridement and antibiotic management, PLA matrices were applied weekly, leading to full closure after 12 weeks. No tendons were lost, and the foot regained full function. Patient 2 is a 47-year-old type 1 diabetic with an open heel ulcer for 2 years. The patient had osteomyelitis and underwent several antibiotic courses. After the last one, PLA matrices were applied to the wound bed, which was fully closed after 7 weeks. No further osteomyelitis episodes were documented. Patient 3 is a 35-year-old female with diabetes, obesity, and an acute plantar wound. Previous wounds on this patient led to non-healing and required amputations, so the we used PLA matrices immediately. Complete closure was obtained after 9 weeks without complications. Patient 4 is a 56-year-old male with a history of heavy smoking ad Lyme disease who underwent a peroneal tendon repair. The post-surgical wound experienced dehiscence and tendon exposure. PLA matrices were used to protect the tendons and promote healing. After 15 weeks , the wound was completely healed, and the foot showed a normal range of motion.
Discussion:
PLA closure matrices induce robust healing in hard-to-heal wounds. Here we illustrate how these matrices can cover bone and tendon structures, maintaining tissue viability and promoting the deposition of granulation tissue on top of it. Furthermore, they can be introduced early in the wound care pathway. They will adapt a fibrous necrotic wound to a granular one that, in turn, can support re-epithelization. The pH modulation of the wound bed environment reduces bacterial load and may prevent infections. Together, it helps preserve tissue integrity and avoid amputations.
Trademarked Items: SupraSDRM
References: 1. Mirhaj M, Labbaf S, Tavakoli M, Seifalian AM. Emerging treatment strategies in wound care. Int Wound J. 2022 Nov;19(7):1934–54.
2. Ring A, Goertz O, Al-Benna S, Ottomann C, Langer S, Steinstraesser L, et al. Accelerated angiogenic induction and vascular integration in a novel synthetic scaffolding matrix for tissue replacement. Int J Artif Organs. 2010 Dec;33(12):877–84.
3. Haller HL, Sander F, Popp D, Rapp M, Hartmann B, Demircan M, et al. Oxygen, pH, Lactate, and Metabolism—How Old Knowledge and New Insights Might Be Combined for New Wound Treatment. Medicina. 2021 Nov;57(11):1190.

.png)