Case Series/Study
(CS-114) Use of Human Reticular Dermis Graft to Heal Ischemic Wounds
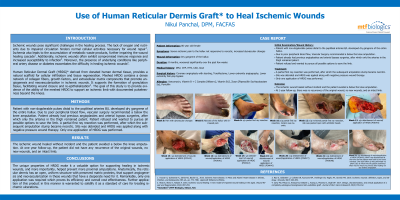
Ischemic wounds pose significant challenges in the healing process. The lack of oxygen and nutrients due to impaired circulation hinders normal cellular activities necessary for wound repair (1). Ischemia also leads to the accumulation of metabolic waste products, further impairing the wound healing cascade (2). Additionally, ischemic wounds often exhibit compromised immune response and increased susceptibility to infection (3). Moreover, the presence of underlying conditions like peripheral artery disease or diabetes exacerbates the difficulty in healing ischemic wounds (2). Human Reticular Dermis Graft (HRDG)* derived from human cadaveric dermal tissue, providing a natural scaffold for cellular infiltration and tissue regeneration. HRDG contains a dense network of collagen fibers, growth factors, and extracellular matrix components that promote angiogenesis and neovascularization in ischemic wounds. It enhances the formation of granulation tissue, facilitating wound closure and reepithelialization (4). The goal of this study is to provide evidence of the HRDG’s ability to heal ischemic wounds. Patient with non-dopplerable pulses developed dry gangrene of the entire hallux. Due to poor peripheral blood flow, Vascular surgery recommended a below the knee amputation. Patient refused and wanted to pursue all possible options to save the limb. A partial first ray resection was performed, after which the subsequent amputation stump became necrotic. Site was debrided and HRDG was applied along with negative pressure wound therapy. Only one application of HRDG was performed.
Methods:
Results: The ischemic wound healed without incident and the patient avoided a below the knee amputation. At one year follow-up, the patient did not have any recurrence of the original wounds, no new wounds, and an intact limb.
Discussion: These unique properties of HRDG make it a valuable option for promoting healing in ischemic wounds, preventing more proximal amputations. Anatomically, the reticular dermis is rich in vascularity, therefore the HRDG results in angiogenesis and neovascularization in these wounds that have a desperate need for it. Further application of this product in this manner is warranted to solidify it as a standard of care for treating ischemic ulcerations.
Trademarked Items:
References: 1.0Younan, G., Guleserian, K., Zahka, K. G., & Backer, C. L. (2016). Ischemic heart disease. In Moss and Adams' Heart Disease in Infants, Children, and Adolescents (9th ed., pp. 772-798). Lippincott Williams & Wilkins.
2. Akita, S., Akino, K., & Yakabe, A. (2016). Ischemic wound healing: A new model of impaired wound healing in the aged. Wound Repair and Regeneration, 24(2), 287-293.
3. Rao, D., Goldstein, L. J., Corbett, D. R., Kavounis, K. M., Voellinger, C. R., Raghu, A. V., ... &
Granick, M. S. (2018). Ischemic wounds: definition, types, and etiology. Wounds, 30(7), 204-209.
4. Carty, M. J., Pribaz, J. J., Antaya, R. J., DeSanti, L., Huang, C., Mooney, D., & Orgill, D. P. (2017). Design, characterization, and clinical application of a completely autologous bioengineered skin-substitute graft. Journal of Burn Care & Research, 38(3), 155-162.

.png)