Case Series/Study
(CS-060) Trichosporon asahii causing Osteomyelitis of the Right Hallux: A Case Report
Methods:
We illustrate a case report where a 78-year-old female patient with peripheral arterial disease and diabetes developed dry gangrenes complicated by osteomyelitis due to Trichosporon asahii in the distal phalange of the right hallux.
Results:
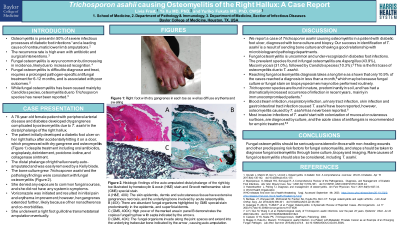
The patient developed a diabetic foot ulcer in her right hallux, which was complicated by dry gangrene and osteomyelitis and progressed over six months despite multiple rounds of empiric oral antibiotics, angioplasty, local wound care, including debridement, betadine, and collagenase ointment. Bone culture after debridement grew Trichosporon asahii. The distal phalange nearly autoamputated and was easily removed by a Kelly blade, which was submitted for pathology examination and showed abundant fungal organisms invading the epidermis, superficial dermis, trabecular bone, and joint spaces on Grocott methenamine silver special stain. She denied any exposure to common sources, and she did not have any systemic symptoms. Voriconazole was initiated for Trichosporon asahii infection. Initially, her pain and erythema improved with voriconazole, however, her gangrenes extended further, likely because of her nonadherence and co-morbidities. She is scheduled for a right foot guillotine transmetatarsal amputation.
Discussion:
Antimicrobial management of diabetic foot infection is critical to prevent major amputations. Although fungal infection is uncommon in diabetic foot infections, it can result in poor wound healing and amputation. Candida species cause fungal osteomyelitis most commonly, followed by Aspergillus species.2 We reported the first case of Trichosporon asahii osteomyelitis in a patient with diabetic foot infection. Fungal osteomyelitis requires pathogen-specific antifungal treatment, and the treatment course tends to be prolonged. Tissue, bone culture, and biopsy need to be considered to guide antimicrobial management when patients with diabetic foot infection do not respond to local wound care or empiric antibiotics.
Trademarked Items:
References: 1. Giurato, L., Meloni, M., Izzo, V., & Uccioli, L. (2017). Osteomyelitis in diabetic foot: A comprehensive overview. World journal of diabetes, 8(4), 135–142. https://doi.org/10.4239/wjd.v8.i4.135
2. Bariteau, J. T., Waryasz, G. R., McDonnell, M., Fischer, S. A., Hayda, R. A., & Born, C. T. (2014). Fungal osteomyelitis and septic arthritis. The Journal of the American Academy of Orthopaedic Surgeons, 22(6), 390–401. https://doi.org/10.5435/JAAOS-22-06-390
3. Castano G, Yarrarapu SNS, Mada PK. Trichosporonosis. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482477/

.png)