Clinical Research
(CR-002) Trial of an Available Technology Dressing for Resource Limited Settings
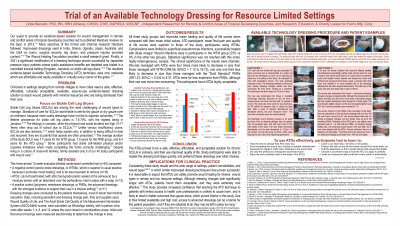
Methods: This three-armed 12-week evaluator-blinded randomized controlled trial compared the improvised Available Technology dressing (ATD) technique (cut-to-fit perforated food-grade plastic with a moisture barrier on the periwound and an absorbent over the perforations) to a negative control (wet-to-moist dressings, equal or superior to usual practice), and a positive control (polymeric membrane dressings). All three protocols were rigorously defined. Dressing changes were conducted by the patients. Data, including wound photos, were collected weekly via WhatsApp, with in-person visits initially and at weeks 1, 4, 8, and 12.
Results:
All three groups saw improvement when compared with their previous usual practice. ATD participants’ pain and quality of life scores were improved over their previous usual practice, and when compared with study participants using wet-to-moist dressings. Participants in the ATD group were far less likely than those in wet-to-moist dressings group to develop wound infections, and their wounds were far more likely to decrease in size. The ATDs were not dramatically inferior to the polymeric membrane dressings, and they were significantly less expensive. The patients found the ATDs acceptable.
Discussion:
ATDs performed well despite the harsh environment. Semi-literate participants could perform dressing changes unaided. The ATDs did not promote infection or clinically significant maceration; they did promote healing, pain relief, and improved quality of life.
Implications for clinical practice: Considering the wide range of settings, patient co-morbidities, and wound types in which this dressing technique has proven successful, it is likely that ATDs can be safely used in other resource-limited situations to promote wound healing. Teaching patients this technique could result in better outcomes than continuing to recommend gauze alone, which is clearly inferior, or advanced dressings, which are likely to be left in place too long (if obtained at all) due to cost constraints.
Trademarked Items:
References: 1. Benskin, L. (2021). A Test of the Safety, Effectiveness, and Acceptability of an Improvised Dressing for Sickle Cell Leg Ulcers in a Tropical Climate (Clinical Trial Registration No. NCT04479618). clinicaltrials.gov. https://clinicaltrials.gov/ct2/show/NCT04479618
2. Benskin, L. 1959-. (2013). Discovering the Current Wound Management Practices of Rural Africans: A Pilot Study [Dissertation, University of Texas Medical Branch]. https://utmb-ir.tdl.org/handle/2152.3/538
3. Benskin, L. L. L. (2013). A review of the literature informing affordable, available wound management choices for rural areas of tropical developing countries. Wound Management and Prevention Journal (OWM), 59(10), 20–41.
4. Bolton, L. L. (2012). Common Nonsense: Rediscovering Moist Wound Healing | Wound Management & Prevention. Wound Management & Prevention Journal. https://www.o-wm.com/blog/common-nonsense-rediscovering-moist-wound-healing
5. Benskin, L. L. (2016). Polymeric Membrane Dressings for Topical Wound Management of Patients With Infected Wounds in a Challenging Environment: A Protocol With 3 Case Examples. Wound Management and Prevention Journal (OWM, 62(6), 42–50. https://www.researchgate.net/publication/304629707_Polymeric_Membrane_Dressings_for_Topical_Wound_Management_of_Patients_With_Infected_Wounds_in_a_Challenging_Environment_A_Protocol_With_3_Case_Examples
6. Toriyabe S, Saito H, Sakurai K. Use of a Food Wrap as a Dressing Material. Advances in Skin and Wound Care. 1999 Oct;12(8):405–6.
7. Takahashi J, Nakae K, Miyagawa M, Yokota O, Fujiki Y, Ide M, et al. Plastic wrap as a dressing material to treat stage III/IV pressure ulcers in the inflammatory phase: a randomized controlled trial. Int J Clin Exp Med. 2017;10(3):5586–94.
8. Tippett A. Does Gauze Have Cause? – Making a Case for Gauze Wound Dressings [Internet]. Wound source: Aletha Tippett MD’s blog. 2012. Available from: https://www.woundsource.com/blog/does-gauze-have-cause-making-case-gauze-wound-dressings
9. Lee YI, Min HG, Kim YL, An SM, Jun S ryung, Choi R ryang. Control Study Evaluating the Efficacy of Wrap Therapy for National Pressure Ulcer Advisory Panel Stage II, III, and IV Pressure Ulcer. Korean Journal of Family Pracice. 2015 Jun 30;5(2):71–6.
10. Bito S, Mizuhara A, Oonishi S, Takeuchi K, Suzuki M, Akiyama K, et al. Randomised controlled trial evaluating the efficacy of wrap therapy for wound healing acceleration in patients with NPUAP stage II and III pressure ulcer. BMJ Open. 2012;2:e000371.
11. Takahashi, J, Yokota O, Fujisawa Y, Sasaki K, Ishizu H, Aoki T, et al. An evaluation of polyvinylidene film dressing for treatment of pressure ulcers in older people. J Wound Care. 2006 Nov;15(10):449–54.
12. Gore MA, Umakumar K, Iyer SP. Polyethylene Surgical Drape Dressing for Split Thickness Skin Graft Donor Areas. In: Gore MA, editor. Skin Grafts [Internet]. InTech; 2013 DOI: 10.5772/54195

.png)