Clinical Research
(CR-029) Closed-Incision Negative-Pressure Wound Therapy for management of donor site after deep inferior epigastric flap
Tripp Holton, MD; Juan Mella-Catinchi, MD; Abdel-Moneim Mohamed, MD; John Oeltjen, MD, PhD; Rita Shelby, MD, MS; Devinder Singh, MD; Dylan Treger, MS; Emily Finkelstein, MD
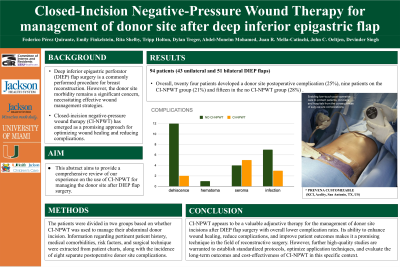
Introduction: Deep inferior epigastric perforator (DIEP) flap surgery is a commonly performed procedure for breast reconstruction. However, the donor site morbidity remains a significant concern, necessitating effective wound management strategies. Closed-incision negative-pressure wound therapy (CI-NPWT) has emerged as a promising approach for optimizing wound healing and reducing complications. This abstract aims to provide a comprehensive review of our experience on the use of CI-NPWT for managing the donor site after DIEP flap surgery.
Methods: Patients that underwent DIEP flap breast reconstruction were selected for retrospective review. Information regarding pertinent patient history, medical comorbidities, risk factors, and surgical technique were extracted from patient charts, along with the incidence of eight separate postoperative donor site complications. The patients were divided in two groups based on whether CI-NPWT was used to manage their abdominal donor incision. IBM SPSS was used for statistical analysis.
Results: Retrospective review identified 94 patients that underwent 43 unilateral and 51 bilateral DIEP flap procedures for breast reconstruction. CI-NPWT was used to manage the donor site in 42 patients while 52 patients had there wound managed with surgical glue.
Overall, twenty four patients developed a donor site postoperative complication (25%), nine patients on the CI-NPWT group (21%) and fifteen in the no CI-NPWT group (28%) .
Fourteen patients developed some level of incisional dehiscence (n=14). Patients with CI-NPWT were significantly less likely to develop this wound complication (p=0.0148) with two patients (n=2) in the CI-NPWT group and twelve (n=12) in the group without it.
Other complications included one hematoma (n=1) on the no CI-NPWT group; nine seroma (n=9) of which 5 were in the CI-NPWT group and 4 in the no CI-NPWT; 10 local infections (n=10) of which 3 were in the CI-NPWT group and 7 in the no CI-NPWT.
Discussion: Based on our experience CI-NPWT appears to be a valuable adjunctive therapy for the management of donor site incisions after DIEP flap surgery with overall lower complication rates. Its ability to enhance wound healing, reduce complications, and improve patient outcomes makes it a promising technique in the field of reconstructive surgery. However, further high-quality studies are warranted to establish standardized protocols, optimize application techniques, and evaluate the long-term outcomes and cost-effectiveness of CI-NPWT in this specific context.
Trademarked Items:
References:
Methods: Patients that underwent DIEP flap breast reconstruction were selected for retrospective review. Information regarding pertinent patient history, medical comorbidities, risk factors, and surgical technique were extracted from patient charts, along with the incidence of eight separate postoperative donor site complications. The patients were divided in two groups based on whether CI-NPWT was used to manage their abdominal donor incision. IBM SPSS was used for statistical analysis.
Results: Retrospective review identified 94 patients that underwent 43 unilateral and 51 bilateral DIEP flap procedures for breast reconstruction. CI-NPWT was used to manage the donor site in 42 patients while 52 patients had there wound managed with surgical glue.
Overall, twenty four patients developed a donor site postoperative complication (25%), nine patients on the CI-NPWT group (21%) and fifteen in the no CI-NPWT group (28%) .
Fourteen patients developed some level of incisional dehiscence (n=14). Patients with CI-NPWT were significantly less likely to develop this wound complication (p=0.0148) with two patients (n=2) in the CI-NPWT group and twelve (n=12) in the group without it.
Other complications included one hematoma (n=1) on the no CI-NPWT group; nine seroma (n=9) of which 5 were in the CI-NPWT group and 4 in the no CI-NPWT; 10 local infections (n=10) of which 3 were in the CI-NPWT group and 7 in the no CI-NPWT.
Discussion: Based on our experience CI-NPWT appears to be a valuable adjunctive therapy for the management of donor site incisions after DIEP flap surgery with overall lower complication rates. Its ability to enhance wound healing, reduce complications, and improve patient outcomes makes it a promising technique in the field of reconstructive surgery. However, further high-quality studies are warranted to establish standardized protocols, optimize application techniques, and evaluate the long-term outcomes and cost-effectiveness of CI-NPWT in this specific context.
Trademarked Items:
References:

.png)