Case Series/Study
(CS-041) Challenging Heel Defect and Skin Graft Utilizing Dehydrated Human Amnion/Chorion Membrane and Negative Pressure Wound Therapy
Full thickness and split thickness skin grafts (STSG) require a healthy granulation bed and sufficient vascularization for success. Patients with underlying comorbidities and poorly vascularized wound locations such as the heel are at risk of skin graft failure.
Methods:
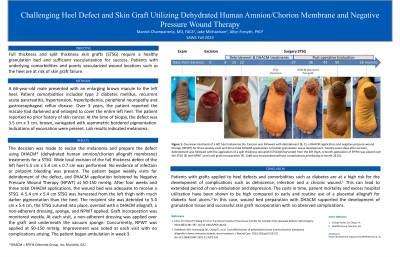
A 66-year-old male presented with an enlarging brown macule to the left heel. Patient comorbidities included type 2 diabetes mellitus, recurrent acute pancreatitis, hypertension, hyperlipidemia, peripheral neuropathy and gastroesophageal reflux disease. Over 3 years, the patient reported the macule had darkened and enlarged to cover the entire left heel. The patient reported no prior history of skin cancer. At the time of biopsy, the defect was 3.5 cm x 3 cm, brown, variegated with asymmetric bordered pigmentation. Indications of excoriation were present. Lab results indicated melanoma.
Results:
The decision was made to excise the melanoma and prepare the defect using DHACM (dehydrated human amnion/chorion allograft membrane) treatments for a STSG. Wide local excision of the full thickness defect of the left heel 5.5 cm x 5.4 cm x 0.7 cm was performed. No evidence of infection or pinpoint bleeding was present. The patient began weekly visits for debridement of the defect, and DHACM application bolstered by Negative Pressure Wound Therapy (NPWT) at 50-150 mmHg. After four weeks, the wound bed was adequate to receive a STSG. A 5.4 cm x 5.4 cm STSG was harvested from the left thigh with much darker pigmentation than the heel. The recipient site was debrided to 5.4 cm x 5.4 cm, the STSG sutured into place, overlaid with a DHACM allograft, a non-adherent dressing, sponge, and NPWT applied. Graft incorporation was monitored weekly. At each visit, a non-adherent dressing was applied over the graft and underneath the vacuum sponge. Concurrently, NPWT was applied at 50-150 mmHg. Improvement was noted at each visit with no complications arising. The patient began ambulation in week 3.
Discussion:
Patients with grafts applied to heel defects and comorbidities such as diabetes are at a high risk for the development of complications.1 This can lead to extended period of non-ambulation and depression. The costs in time, patient mortality and excess hospital utilization can be high compared to early and routine use of placental allografts for post-surgical defects.2 In this case, wound bed preparation with DHACM supported the development of granulation tissue and successful skin graft incorporation with no observed complications.
Trademarked Items:
References: 1.Chou CY, Chiao HY, Wang CY, et al. Functional results of free tissue transfer for complex heel-calcaneal defects. Microsurgery. 2018;38(4):381-387.
2.Tettelbach WH, Armstrong DG, Chang TJ, et al. Cost-effectiveness of dehydrated human amnion/chorion membrane allografts in lower extremity diabetic ulcer treatment. J Wound Care. 2022;31(Sup2):S10-S31.

.png)