Case Series/Study
(CS-062) Wound Management for Prolonged Mpox Skin Lesions in a Patient with Advanced HIV/AIDS
Although mpox became a public health emergency of international concern by the World Health Organization in 2022, wound care management for mpox skin lesions have not been established yet.
Methods:
We illustrate a case report where a 43-year-old male patient with advanced HIV developed severe mpox skin lesions that required intense wound care management.
Results:
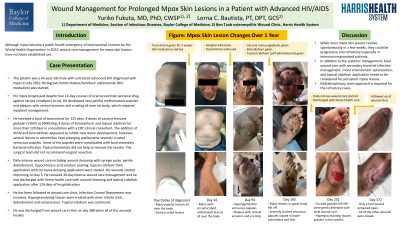
The patient was a 43-year-old male with untreated advanced HIV who was diagnosed with mpox in July 2022. Antiretroviral therapy was started in August 2022. His mpox progressed despite two 14-day courses of oral tecovirimat. He developed very painful erythematous papules and plaques with central erosions and crusting all over his body, which required inpatient management.
He received a total of tecovirimat for 125 days, 9 doses of vaccina immune globulin (VIGIV) at 9000U/kg, 4 doses of brincidofovir and topical cidofovir for more than 120 days in consultation with a CDC clinical consultant. The addition of VIGIV and brincidofovir appeared to inhibit new lesion development; however, several lesions in extremities kept enlarging and became severely crusted verrucous papules. Some of the papules were complicated with local secondary bacterial infection. Topical keratolytic did not help to remove the keratin. The surgical team did not recommend surgical resection. Daily intense wound care including wound cleansing with syringe pulse, gentle debridement, hypochlorous acid solution soaking, topical cidofovir thick application with occlusive dressing application were started. His wounds started improving on day 3. He was discharged with home health care with wound cleansing and topical cidofovir application after 20-day intense wound care management. He has been followed at wound care clinic. Hypergranulating tissues were treated with silver nitrate stick, debridement and compression. Most lesions have healed and the three remaining lesions have been getting smaller.
Discussion:
While most mpox skin lesions resolve spontaneously in a few weeks, they could be progressive and refractory especially in immunocompromised patients. In addition to the systemic management, local wound care with secondary bacterial infection management, moist environment optimization, and topical cidofovir application needs to be considered for persistent mpox lesions.
Trademarked Items:
References: Shamim MA, Padhi BK, Satapathy P, Veeramachaneni SD, Chatterjee C, Tripathy S, Akhtar N, Pradhan A, Dwivedi P, Mohanty A, Rodriguez-Morales AJ, Sah R, Al-Tammemi AB, Al-Tawfiq JA, Nowrouzi-Kia B, Chattu VK. The use of antivirals in the treatment of human monkeypox outbreaks: a systematic review. Int J Infect Dis. 2023 Feb;127:150-161. doi: 10.1016/j.ijid.2022.11.040. Epub 2022 Dec 5. PMID: 36470502; PMCID: PMC9719850.
Pettit NN, Imam S, Sherer R, Hazra A. Treatment options for severe or refractory mpox virus infection in patients with advanced HIV. Int J STD AIDS. 2023 May;34(6):366-373. doi: 10.1177/09564624231152940. Epub 2023 Jan 28. PMID: 36708269.
Rubio-Muniz CA, Montero-Menárguez J, López-Valle A, Agud-Dios M, Arroyo-Andrés J, Rodriguez-Peralto JL, Palencia-Pérez SI, Tarín-Vicente EJ. Monkeypox: is topical cidofovir a good idea? Clin Exp Dermatol. 2023 Feb 2;48(2):132-134. doi: 10.1093/ced/llac038. PMID: 36730511.

.png)