Practice Innovations
(PI-005) Wear Time and Ease of Use of a Transparent Gel Dressing for Prevention of Sacral Pressure Injury
Introduction: Foam and gel dressings are often used to protect against pressure injuries (PIs) however, they must be removed to evaluate the condition of the skin.1 Repetitive removal of adhesive foam dressings can weaken the skin integrity thereby adding to the risk of PIs or risk of medical adhesive related skin injury (MARSI).2 Compliance with patient repositioning can also help to protect the skin against PIs however, it is not always reliable.3
Methods:
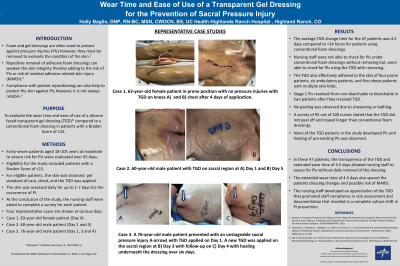
Methods: Forty seven patients aged 18-105 years at high-risk for PIs were evaluated over 65 days. A subset of patients (n=12) received a silicone foam dressing for the treatment of full-thickness PIs. Eligibility for the study included patients with a Braden Score of ≤15. For eligible patients, the sacral region of the skin was cleaned and dried and the TGD was applied. The skin was assessed daily for up to 1-8 days for the occurrence of PI in the sacral region.
Results:
Results: The average TGD change time was 4.5 days compared to historically recorded 2.5 days for patients using conventional foam dressings. Stage 1 PIs resolved from non-blanchable to blanchable in two patients. A survey of 95 out of 100 nurses stated that the TGD did not peel off and stayed longer than conventional foam dressings. No peeling of the TGD was observed even for patients that showered or bathed. The TGD also effectively adhered to the skin of four prone patients, six ambulatory patients, and five obese patients with multiple skin folds. Furthermore, the nursing staff developed an appreciation of the TGD that promoted staff compliance in skin assessment and documentation that resulted in a complete culture shift in PI prevention.
Discussion: We conclude from this study that a TGD can be used to prevent sacral PIs in acute care patients with Braden Scores of ≤15. The transparency of the TGD allowed nursing staff to assess for PIs without daily removal of the dressing. Compliance in documentation increased of q-shift skin assessments and two-person skin assessments upon admission and transfers. Improved collaboration between the wound care department and nursing for skin related issues.
Trademarked Items:
References:
References:
1. Haesler, E, European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. EPUAP/NPIAP/PPIA. 2019.
2. Fumarola, S., Allaway, R., Callaghan, R., Collier, M., Downie, F., et al Overlooked and underestimated-medical adhesive-related skin injuries. Best practice consensus document on prevention. J Wound Care, 2020. 29(Sup3c): p. S1-S24
3. Yap TL, Kennerly SM, Ly K. Pressure Injury Prevention: Outcomes and Challenges to Use of Resident Monitoring Technology in a Nursing Home. J Wound Ostomy Continence Nurs. 2019 May/Jun;46(3):207-213. doi: 10.1097/WON.0000000000000523.

.png)