Case Series/Study
(CS-020) Utilization of Transforming Powder Dressing for Managing Peristomal Wound and Mucus Fistula in a Neonate after Omphalocele Repair
Omphalocele is a congenital condition where a portion of the intestine protrudes through the abdominal wall near the navel, affecting approximately 1 in 4,200 births in the United States. The current standard of care involves surgical intervention, including the application of a silo pouch to contain the omphalocele, followed by repair and ostomy creation. However, complications such as wound infection, delayed healing, fascial separation, patient discomfort, and loss of abdominal domain can occur. Novel approaches to optimize wound healing, minimize dressing changes, and alleviate associated pain are needed. In this case study, we present the application of an extended wear transforming powder dressing (TPD), composed of polymers similar to those found in contact lenses, to expedite wound healing and improve patient care options.
Methods:
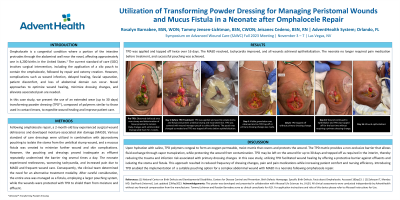
Following omphalocele repair, the neonate experienced surgical wound dehiscence and developed moisture-associated skin damage (MASD). Various standard of care dressings were utilized in combination with jejunostomy pouching to isolate the stoma from the umbilical stump wound, and a mucus fistula was created to minimize further wound and skin complications. However, the pouching and dressings proved inadequate as effluent repeatedly undermined the barrier ring multiple times a day. The neonate experienced restlessness, worsening tachycardia, and increased pain due to MASD and frequent wound care. Consequently, the clinical team determined the need for an alternative treatment modality. After careful consideration, the entire area was managed as a fistula, employing a larger pouching system, while the wounds were protected with TPD to shield them from moisture and effluent.
Results:
Over a span of 19 days, a total of three applications of TPD were administered. The MASD resolved, tachycardia improved, and all wounds achieved epithelialization. The neonate no longer required pain medication before treatment, and successful pouching was achieved.
Discussion:
Introducing TPD provided a suitable pouching option for a complex abdominal wound and MASD in a neonate following omphalocele repair. Utilizing TPD facilitated wound healing by offering a protective barrier against effluent without the need for stoma isolation. This approach resulted in reduced frequency of dressing changes, leading to decreased patient discomfort and pain.
Trademarked Items: Altrazeal® Transforming Powder Dressing
References:

.png)
