Case Series/Study
(CS-145) Utilization of Omega 3 Fish Skin Graft In The Case of Surgical Dehiscence of A 1st MPJ Arthrodesis with Associated Osteomyelitis
Methods:
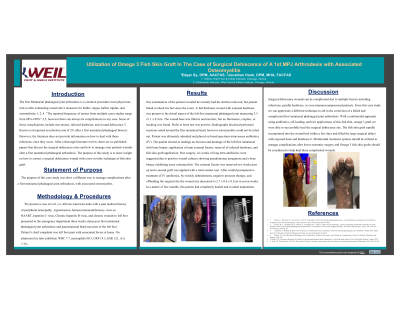
61yo African American male with a PMH of peripheral neuropathy, HIV, hepatitis C, Chronic hepatitis B virus presented to the ED three weeks s/p 1st MPJ arthrodesis and panmetatarsal head resection. Patient’s CC was left foot pain with associated fevers at home. On admission labs exhibited: WBC 7.7, neutrophils 80.3, CRP 19.5, ESR 121, A1c 7.3%.
Results: Our examination of the patient revealed he recently had his stitches removed, but patient failed to check his feet since. A full thickness wound with exposed hardware was present to the surgical site measuring 3.5 x1.1 x 0.3cm. The wound base was fibrotic and necrotic, but no fluctuance, crepitus, or tracking found. Probe to bone test was positive. Radiographs disclosed periosteal reactions noted around the metatarsal head. Patient was admitted and placed on broad spectrum intravenous antibiotics. The patient underwent incision and drainage of the first metatarsal with bone biopsy, application of mini external fixator, removal of infected hardware, and fish skin graft application. 6 weeks of antibiotics were suggested due to positive wound cultures showing pseudomonas aeruginosa and a bone biopsy exhibiting acute osteomyelitis. The external fixator was removed two weeks post-op and a second graft was applied with a total contact cast. After careful postoperative treatment of IV antibiotics, bi-weekly debridements, negative pressure therapy, and offloading the surgical site the wound size decreased to 2.7 x 0.6 x 0.2cm in seven weeks. In a few months, this patient had completely healed and avoided amputation.
Discussion:
Surgical dehiscence can be complicated due to multiple factors including infections, or even immunocompromised patients. This case study a different technique to aid in the correction of a failed first MPJ arthrodesis. A multimodal approach using antibiotics, off-loading, and two applications of fish skin graft was able to successfully heal the dehiscence site. The fish skin graft rapidly incorporated into the wound bed within a few days and filled the large surgical defect with exposed bone and hardware. Multimodal treatment options should be utilized to manage complications after lower extremity surgery.
Trademarked Items:
References: 1. Harris, E., Moroney, P., & Tourné, Y. (2017). Arthrodesis of the first metatarsophalangeal joint—A biomechanical comparison of four fixation techniques. Foot and Ankle Surgery, 23(4), 268–274. doi: 10.1016/j.fas.2016.07.005
2. Korim, M. T., Mahadevan, D., Ghosh, A., & Mangwani, J. (2017). Effect of joint pathology, surface preparation and fixation methods on union frequency after first metatarsophalangeal joint arthrodesis: A systematic review of the English literature. Foot and Ankle Surgery, 23(3), 189–194. doi: 10.1016/j.fas.2016.05.317
3. Anderson JJ, Hansen M, Rowe GP, Swayzee Z. Complication rates in diabetics with first metatarsophalangeal joint arthrodesis. Diabet Foot Ankle. 2014;5:10.3402/dfa.v5.24649. Published 2014 Jun 27. doi:10.3402/dfa.v5.24649
4. Roukis T,S. First Metatarsal-Phalangeal Joint Arthrodesis: Primary, Reviesion, and Salvage of Complications. Clinics in Podiatric Medicine and Surgery. July 2017
5. Roukis T,S. Salvage arthrodesis for failed first metatarsophalangeal joint arthroplasty: A network meta-analysis. Foot and Ankle Surgery. August 2019.
5. Trinh TT, Dünschede F, Vahl CF, Dorweiler B. Marine Omega3 wound matrix for the treatment of complicated wounds. Phlebologie. 2016;45(2):93-98.

.png)