Case Series/Study
(CS-065) The Use of an Autologous Multilayered Leukocyte, Platelet and Fibrin Patch for Diabetic Ulcers: Shifting the Mindset
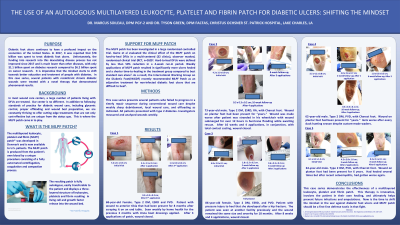
Diabetic foot ulcers continues to have a profound impact on the economics of the United States. In 2017, it was reported that $78 billion was used to treat diabetic foot ulcers. Unfortunately, the funding into research into this devastating disease process is much lower than others, with only $1.1 billion spent on diabetes research but $6.2 billion spent on cancer research. It is imperative that the mindset starts to shift towards better education and treatment of people with diabetes. In this case series, several patients with recalcitrant chronic diabetic wounds were treated with an autologous multilayered leukocyte, platelet, and fibrin(MLPF) patch and demonstrated phenomenal results.
Methods:
The study presents several patients who failed to progress in a timely repair sequence during conventional wound care despite weekly sharp debridement, local wound care, and offloading as indicated. All patients presented with type 2 diabetes. Investigators measured and analyzed wounds weekly.
Results: The first patient, a 68-year-old female with ESRD and PVD presented with a wound to the anterior tibia that has been present for 8 months. She previously had been seen weekly by home health with Unna boots applied. In the wound center, MLPF patches were applied and dramatically decreased the size of her wound in just three applications. The second patient, a 73-year-old male with ESRD, RA and significant Charcot deformity presented with a wound to the plantar foot that has been present for “years”. After 10 weeks and just four applications of the MLPF patch, the patient’s wound was healed. A third patient, an 86-year-old female with ESRD and PVD presented with a pressure injury on her heel that developed after she broke her hip. The wound had not demonstrated any improvement in over 18 months. With four applications and just 8 weeks, the wound went on to heal completely. A fourth patient, with peripheral vascular disease and significant Charcot deformity, presented with a wound that had been present for over 6 years with intermittent healing noted. In eight weeks and after six applications of the MLPF patch, the wound completely closed.
Discussion:
In this case series, the use of the autologous patch, in conjunction with diabetes management, local sharp debridement and appropriate offloading, contributed to significant improvement in the wounds. With this shift in mindset, of using the patient’s own ability to heal, patients demonstrated improved healing, therefore changing the way this clinic treats their patients with diabetes.
Trademarked Items: 3C Patch
References:

.png)