Case Series/Study
(CS-003) Reducing Veteran Hospital Resource Utilization for Treatment of Complex Post-Operative Vascular Wounds: Case Series Using Novel Transforming Powder Dressing
Increasing healthcare costs, shortages in healthcare resources, and an aging population with multiple comorbidities have made wound management a growing clinical, economic, and social burden, necessitating a paradigm shift in current standard of care (SOC) therapies.1 Medicare cost estimates for acute and chronic wound treatment in the United States (US) range from $28.1 billion to $96.8 billion annually.2 The US Veteran’s Affairs Medical Center treats an increasingly aging population predisposed to nonhealing vascular wounds in the setting of multiple comorbidities. We present a case series of 4 patients with complex post-operative vascular wounds treated with a novel transforming powder dressing (TPD) and report findings related to wound healing and resource utilization compared to SOC.
Methods:
Four patients with complex wounds of differing etiologies resulting from sequela of severe vascular pathology were assessed. Each patient was observed to have comorbidities with a history of poor wound healing requiring consideration of alternate treatment modalities. All patients were converted to treatment with TPD, and dressings were changed based on clinical necessity. The wound closure progress was monitored along with resource utilization compared to SOC.
Results:
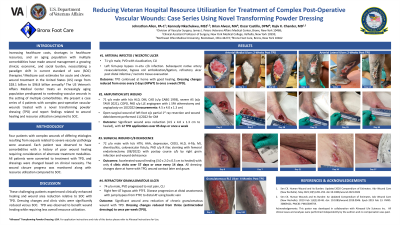
1. Arterial infected/necrotic ulcer: 71 y/o male, PVD with claudication, and CLI
Outcome: TPD used at home for 14 days with enhanced wound healing. Dressing changes reduced from 3x/week (NPWT) to once weekly (TPD).
2. Refractory granulomatous ulcer: 74 y/o male, PVD, rest pain, and CLI
Outcome: Significant wound area reduction with TPD over 120 days. Dressing changes reduced from 3x/week (various antimicrobial dressings) to once weekly (TPD).
3. Amputation: 71 y/o male, DM, CAD, severe AS, and multiple comorbidities.
Outcome: Wound healed in 85 days with weekly TPD applications versus 3x/week (NPWT).
4. Surgical Wound: 72 y/o male, HTN, and multiple comorbidities with postop course c/b by groin infection and wound dehiscence.
Outcome: TPD utilized weekly and wound healed in 57 days, requiring only 4 clinic visits.
Discussion:
These challenging patients experienced clinically enhanced healing and wound area reduction relative to SOC with TPD. TPD may provide the benefit of promoting wound healing while requiring less overall resource utilization due to need for fewer dressing changes compared to SOC.
Trademarked Items:
References: 1. Sen CK. Human Wound and Its Burden: Updated 2020 Compendium of Estimates. Adv Wound Care (New Rochelle). May 2021;10(5):281-292. doi:10.1089/wound.2021.0026
2. Sen CK. Human Wounds and Its Burden: An Updated Compendium of Estimates. Adv Wound Care (New Rochelle). 2019 Feb 1;8(2):39-48. doi: 10.1089/wound.2019.0946. Epub 2019 Feb 13. PMID: 30809421; PMCID: PMC6389759.

.png)