Evidence-Based Practice
(EBP-003) The use of a pure Hypochlorous Acid (pHA) based cleanser in a standardized way in an inpatient setting by a WOC nursing service. Also, what is in the canister with pHA instillation with NPWT?
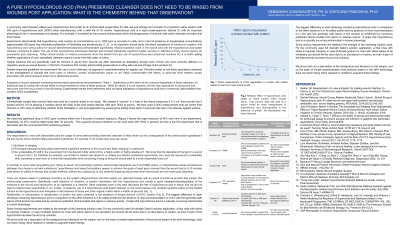
Consensus guidelines encourage the standardized use of tissue safe cleansers that are effective in removing biofilms and necrotic tissue. In our inpatient practice, it is common for us to reach for a pHA based cleanser. This cleanser is applied to a wound with frequent soaks via a gauze. Another way to manage these wounds, is to use the pHA cleanser in an instillation mode. The necrotic material is removed effectively, and its removal is evidenced not only visually in the wound, but also by the appearance of the suspended necrotic tissue in the collection canister.
Methods:
We attempted to study the “extent of usage” of pHA. Thus over a period of five months, we prospectively recorded the wound healing journey of each patient who was treated with pHA while in our inpatient care. We monitored wound progress via reduction in wound size (particularly with negative pressure wound therapy), length of therapy, and appearance of healthy granulation tissue. We present here the details of these patients and their wounds who were treated with pHA. We also present three notable cases, and also visual images of the canister contents to indicate where the necrotic matter ended up post-cleansing with pHA.
Results:
This study involved the treatment of 20 patients over the course of 5 months, with 3 notable cases. There were no adverse events related to product use and the case details presented showed steady healing progress with pHA. Images of the canisters show that while the necrotic tissue vanished over time from the wound, it appeared as a cloudy, suspended matter in the canisters. These observations prove that pHA with instillation works to remove necrotic tissue. It is also expected to decontaminate the wound via biofilm removal.
Discussion: The use of hypochlorous acid based cleanser is a safe and widespread practice, in our hospital. The ability of the product to remove necrotic tissue is remarkably visible when it is used in conjunction with the use of instillation and NPWT with dwell time.
Trademarked Items: Vashe, Veraflo
References: 1. Armstrong DG, Bohn G, Glat P, Kavros SJ, Kirsner R, Snyder R, Tettelbach W.Armstrong DG, et al. Expert Recommendations for the Use of Hypochlorous Solution: Science and Clinical Application. Ostomy Wound Management 2015 May;61(5): S2-S19. https://pubmed.ncbi.nlm.nih.gov/28692424/
2. Dissemond J. Wound Cleansing: benefits of hypochlorous acid. Journal of Wound Care Published Online:5 Oct 2020https://www.karger.com/Article/Abstract/481545
3. Robson MC. Advancing the science of wound bed preparation for chronic wounds. Ostomy Wound Manag. 2012;58(12):2–3. https://www.o-wm.com/article/pearls-practice-advancing-science-wound-bed-preparation-chronic-wounds
4. Sakarya S, Gunay N, Karakulak M, Ozturk B, Ertugrul B. Hypochlorous acid: an ideal wound care agent with powerful microbicidal, antibiofilm, and wound healing potency. Wounds 2014;26(12):342–350. https://pubmed.ncbi.nlm.nih.gov/25785777/
5. Robson MC, Payne WG, Ko F, Mentis M, Donati G, Shafii SM, Culverhouse S, Wang L, Khosrovi B, Najafi R, Cooper DM, Bassiri M. Hypochlorous Acid as a Potential Wound Care Agent: Part II. Stabilized Hypochlorous Acid: Its Role in Decreasing Tissue Bacterial Bioburden and Overcoming the Inhibition of Infection on Wound Healing. J Burns Wounds. 2007 Apr 11;6:e6. https://pubmed.ncbi.nlm.nih.gov/17492051/

.png)