Practice Innovations
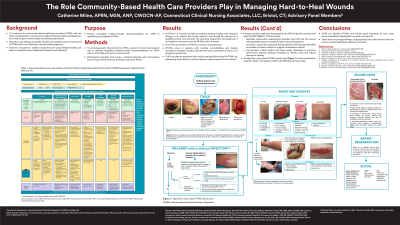
(PI-016) The Role Community-Based Health Care Providers Play in Managing Hard-to-Heal Wounds
Introduction
It is common for community-based healthcare providers (CHPs)—non-specialists in wound care—to deliver initial and ongoing management for a wide range of wound types and diverse populations. Wounds in any setting can rapidly transition to a stalled, hard-to-heal wound (HTHW) that is not following a normal healing trajectory.1 Failure to recognize or address issues that can cause delayed healing can lead to increased costs, healthcare utilization and suffering.2
Methods:
Methods
To encourage early intervention by CHPs, a panel of wound care experts set out to develop actionable evidence-based recommendations for CHPs delineating characteristics and appropriate care in identifying and treating HTHWs.
Results:
Results
· A HTHW is a wound that fails to progress towards healing with standard therapy in an orderly and timely manner and should be referred to a qualified wound care provider (QWCP) for advanced assessment and diagnosis if not healed or reduced in size by 40-50% within 4 weeks.3
· HTHWs occur in patients with multiple comorbidities, and display increases in exudate, infection, devitalised tissue, maceration or pain, or no change in wound size.
· CHPs can play an important initial role by seeing the individual’s HTHW risk, addressing local infection, and providing an optimal wound environment.4
o The wound and periwound should be cleansed with a non-cytotoxic antiseptic or pH-balanced surfactant solution post regional skin hygiene.5
o If appropriate, prompt wound debridement with gauze or a soft pad is recommended.
o For draining wounds, the periwound should be protected with a barrier product.
o When increased risk of a HTHW is identified, healing is delayed, or infection is suspected, a topical antimicrobial/antiseptic agent should be used.
o For highly draining wounds, a superabsorbent/gelling fiber dressing is recommended.
o Alginate or foam dressings are recommended for wounds with medium drainage, and hydrocolloid, sheet hydrogel or thin foam dressings for minimal drainage.
o A basic toolkit for wound care should include antiseptic/surfactant wound/skin cleansers, debridement products, a barrier product to protect the periwound, a selection of absorptive dressings appropriate to the level of exudate observed to ensure a moist wound environment, and a secondary cover dressing if needed.
Discussion:
Discussion
CHPs who refer early and strengthen their ability to deliver good evidence-based wound care can greatly improve overall healthcare efficiency and cost.
Trademarked Items:
References:
References:
1. Milne J, Searle R, Styche T. The characteristics and impact of hard-to-heal wounds: results of a standardised survey. J Wound Care 2020;29:282-288.
2. Vowden P. & Vowden K. The economic impact of hard-to-heal wounds: promoting practice change to address passivity in wound management. Wounds Int 2016;7:10-15.
3. Atkin L, Bucko Z, Conde Montero E, Cutting K, Moffatt C, Probst A, et al. Implementing TIMERS: the race against hard-to-heal wounds. J Wound Care. 2019;23(Suppl 3a):S1-S50.
4. Swanson T, Ousey K, Haesler E, et al. (2022) International Wound Infection Institute (IWII) Wound Infection in Clinical Practice. Wounds International.

.png)
