Laboratory Research
(LR-003) The Importance of Flow through an NPWT Dressing for Proper Exudate and Negative Pressure Management
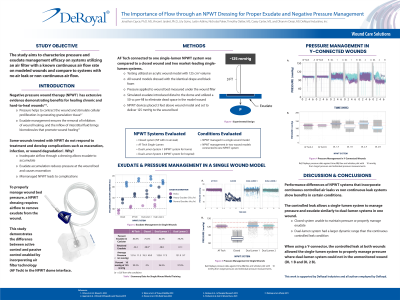
Negative pressure wound therapy (NPWT) has extensive evidence demonstrating benefits for healing chronic and hard-to-heal wounds. However, some wounds do not improve and suffer from complications such as maceration or wound degradation. These complications often occur when an NPWT system fails to appropriately manage exudate reducing negative pressure delivered to the wound1. Proper exudate and pressure management require airflow to remove fluid from the system effectively and ensures the prescribed pressure reaches the wound bed. This study aims to characterize pressure and exudate management efficacy utilizing an air filter with a known air flow rate compared to dressings without air leaks (closed condition) connected to single and double-lumen NPWT systems.
Methods:
The study evaluates a dome incorporating an air filter (dome-air filter) to facilitate exudate removal and pressure management in model wounds configured in a closed condition. Conditions evaluated included the dome-air filter, the closed control condition, and dressings connected to two standard multi-lumen NPWT devices placed 3 feet above modeled wounds under 125 mmHg negative pressure. We primed the systems with 170 mL of simulated exudate followed by a rate of 4 mL/hr, the maximum exudate rate for home use, for 16 hrs. Each condition was tested in triplicate.
We evaluated exudate management by weighing the wound model and canister before, 20 minutes, 1 hour, and 16 hrs. Manometers connected below the dome monitored pressure at 10Hz. Repeated measures ANOVA with post-hoc Wilks test identified significant differences in exudate management. Descriptive statistics and 99.7% (3σ) confidence intervals (CI) compared pressure management between systems.
Results:
Repeated measures ANOVA demonstrated a significant difference in the canister (p=0.019) and dressing fluid volumes (p = 0.011). Post-hoc testing showed a significant difference between the closed condition and each remaining condition (p < 0.05). Exudate removal for each condition was as follows: 83.9% dome-air filter, 82.4% multi-lumen system 1, 78.3% for multi-lumen system 2, and 75.4% for the closed condition. The dome-air filter single-lumen system managed pressure effectively at 121.6±7.0 mmHg (99.7% CI) with similar efficiency to multi-lumen system 1 (122.8±14.7 mmHg) and 2 (121.9±10.31 mmHg).
Discussion: This study demonstrates that a dome-air filter can enable a single-lumen NPWT device adequately control wound site pressure and exudate comparable to multi-lumen systems. In addition, these results demonstrate the need for consistent and controlled airflow through an NPWT dressing to support efficient exudate removal and tighter pressure management during therapy.
Trademarked Items:
References: 1-Int. Wound Journal 2021 20(2):328-344

.png)