Clinical Research
(CR-022) The Implementation of a Comprehensive Wound Care Program Powered by A Digital Wound Platform to Decrease Hospital Acquired Pressure Injuries Incidence Rate
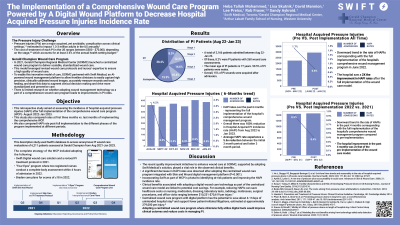
A regional medical center in the US adopted a holistic wound care program (WCP) that included a digital wound care solution (DWCS) to improve pressure injury care. This retrospective study compared the incidence of hospital-acquired pressure injuries (HAPI) before and after implementing the comprehensive WCP. HAPI rate post-full implementation was also compared to the different phases of the program implemented at different periods.
Methods:
The complete strategy of the WCP included adopting the following:
A DWCS in Q4, 2021.
A revised PI treatment protocol in Q4, 2021.
Four eyes program where two registered nurses conduct a complete body assessment within 4 hours of admission in Q1, 2022.
Braden care plans for scores of ≤18 in Q3, 2022.
The study used the DWCS database to access and compare 6,211 anonymous PI evaluation data across different point from from Aug 2021-Jan 2023.
Results:
The study showed a significant decrease in HAPI rates after adopting the WCP (P< 0.001). The incidence rate decreased by 4.2% six months after the full implementation- (August 2022- Jan 2023). Further, a 5.6x reduction in the HAPI rate was observed between the initial three months (Aug-Oct 2022) and the last 3-months of full program implementation (Nov 2022-Jan 2023).
A reduction in the HAPI incidence rate was recorded, with an overall improvement following the full implementation of the WCP (August 2022- Jan 2023) of 56% compared to pre-periods (Sept-Dec 2021) and 53% compared to Nov 2021-May 2022.
Discussion:
Incorporating a DWCS as part of WCP is pivotal to identifying at-risk patients and improving the HAPI incidence rate. Reducing HAPI can save healthcare costs on nursing, medication, dressing, laboratory tests, radiology, mattresses, surgical procedures, and office visits ranging between $10,231- $70,619 per injury.1 It has the potential to save about 4-11 days of unintended hospital stay2 and support fewer patient-initiated litigations, estimated at approximately 279,000 per injury.3
Trademarked Items:
References: Brem H, Maggi J, Nierman D, Rolnitzky L, Bell D, Rennert R, Golinko M, Yan A, Lyder C, Vladeck B. High cost of stage IV pressure ulcers. Am J Surg. 2010 Oct;200(4):473-7. doi: 10.1016/j.amjsurg.2009.12.021.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2950802/
Graves N, Birrell F, Whitby M. Effect of pressure ulcers on length of hospital stay. Infect Control Hosp Epidemiol. 2005;26(3):293-7. doi: 10.1086/502542. PMID: 15796283.
Gefen A, Kolsi J, King T ,et al. Modeling the cost-benefits arising from technology-aided early detection of pressure ulcers. Wounds International.2020; 11(1):22:29

.png)