Case Series/Study
(CS-036) Risk Mitigation by Avoiding the Operating Room: Wound Closure in High Surgical Risk Patients Using an Innovative Bioactive Glass Matrix.
The American Society of Anesthesiologists (ASA) physical status classification was developed to help predict operative risk on a scale of 1-5, whereby 1 is normal health and 5 is moribund.1 Recent data has shown that patients with an ASA class of IV or greater are 17 to 63 times more likely to develop a medical complication and 212 to 2093 times more likely to die following surgery.1
Many of the same co-morbidities associated with severe systemic disease and increasing ASA class/risk, are also markers of patients at high risk for development of chronic wounds. Thus, many patients being treated for chronic wounds are poor candidates for surgical intervention. As a result wound management decisions in these high-risk patients is challenging.
A recently developed bioactive glass wound matrix* (BGWM) has demonstrated promise in wound care.2 This bioactive glass nanofiber has been shown to stimulate soft tissue growth and angiogenesis, and to reduce inflammation and incidence of infection.3-5 Here we present a series of patients with large chronic wounds that were referred to a surgical office for operative intervention. To mitigate high surgical risk, these patients were all treated in the outpatient clinic with BGWM.
Methods:
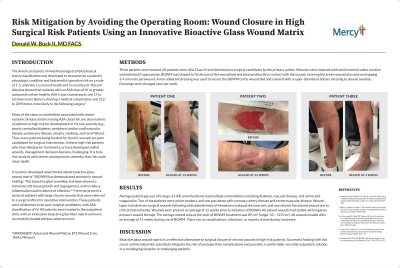
Three patients were treated. All patients were ASA Class IV and deemed poor surgical candidates by the primary author. Wounds were cleansed with saline and debrided if appropriate. BGWM was shaped to fit the size of the wound bed and placed in direct contact with the wound surface. A non-adherent dressing was used to secure the BGWM to the wound bed and covered with a bolster dressing to absorb exudate. Dressings were changed once per week.
Results:
Average patient age was 69 (range: 61-84) and all patients had multiple comorbidities including diabetes, vascular disease, and active anti-coagulation. Wounds were present an average of 12 weeks prior to initiation of BGWM. The average wound area at the start of BGWM treatment was 89 cm2 (range: 33 – 119 cm2). All wounds healed after an average of 11 weeks (range: 3 – 14) during use of BGWM. There were no complications, infections, or reports of pain during treatment.
Discussion:
BGWM is an effective alternative to surgical closure of chronic wounds in high-risk patients. Successful wound closure with this novel, synthetic skin substitute mitigates the risk of postoperative complications and provides a comfortable, versatile outpatient solution to a challenging situation in challenging patients.
Trademarked Items:
References: 1. Hackett NJ, De Oliveira GS, Jain UK, Kim JYS. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg, 2015;18:184-190.
2. Milne J, Searle R, Styche T. The characteristics and impact of hard-to-heal wounds: results of a standardized survey. J Wound Care 2020;29:282-288.
3. Armstrong DG, Orgill DP, Galiano RD, et al. A multi-centre, single-blinded randomised controlled clinical trial evaluating the effect of resorbable glass fibre matrix in the treatment of diabetic foot ulcers. Int Wound J. 2022 May;19(4):791-801.
4. Jung S, Day T, Boone T, et al. Anti-biofilm activity of two novel, borate based, bioactive glass wound dressings. Biomed. Glasses 2019; 5:67–75.
5. Rahaman MN, Day DE, Bal BS, et al. Bioactive glass in tissue engineering. Acta Biomater. 2011; 7(6): 2355–2373.

.png)