Case Series/Study
(CS-027) Inflammation Relief Provides Key to Healing for Four Young People with Pyoderma Gangrenosum
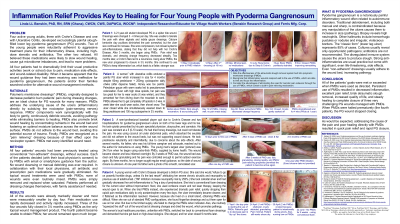
Pyoderma gangrenosum is a notoriously painful inflammatory wound often related to autoimmune disorders which tends to increase in size (pathergy) when it is debrided or manipulated in any way. Four active young adults with Inflammatory Bowel Diseases (IBD) developed excruciatingly painful slough-filled lower leg pyoderma gangrenosum (PG) wounds. All of the patients were wary of using aggressive high-dose steroids and antibiotics to manage their inflammatory illness. They were concerned that these treatments could cause gut microbiome imbalances and make their ulcers worse.
All four patients had to limit their usual productive activities (work or school) due to pain, medication side effects, and wound-related disability. When it became apparently that their health care providers were unfamiliar with effective wound management methods for PG, the patients and/or their families searched online for alternative treatments.
Methods:
Polymeric membrane dressings (PMDs) relieve pain and address the underlying cause of the ulcers (inflammation) directly by subduing the nociceptor (pain-sensing nerves) response. PMDs’ components work synergistically with the body to gently continuously debride wounds, avoiding pathergy while eliminating barriers to healing. PMDs also promote brisk wound healing by concentrating nutrients in the wound bed and fostering an ideal moisture balance across the entire wound surface. PMDs do not adhere to the wound bed, avoiding this potential source of trauma.
Each of the patients decided (with their local physician’s consent) to try PMDs with email or smartphone guidance from the author. Patients/families performed all dressing changes themselves. No wound cleansing or manual debriding was ever required. In collaboration with their local physicians, antibiotic and prescription pain medications were gradually eliminated.
Results:
All four wounds were markedly cleaner and most were measurably smaller already by day four. Pain medication use rapidly decreased and activity rapidly increased. Three of the four wounds fully closed in 3½ months using PMDs as the only topical wound treatment. The fourth patient became unable to obtain PMDs; her wound remained open for many more months.
Discussion:
Persistent use of PMDs resulted in decreased inflammation, excellent pain relief, brisk atraumatic slough removal, increased quality of life, and steady healing to complete closure of three very challenging PG wounds managed with PMDs. When PMDs were halted prematurely (the fourth patient), the PG wound stopped closing.
Trademarked Items:
References: 1. Hubbard, M. (2006, June). Pyoderma gangrenosum and the use of polymeric membrane dressings. Poster #139 presented at the 38th Annual Conference of the WOCN Society, Minneapolis, MN. USA
2. Sessions R. (2009, June). Can a drug-free dressing decrease inflammation and wound pain? What does the evidence say? Poster #3436 presented at the 41st Annual Conference of the WOCN Society, St. Louis, MO. USA
3. Wollina, U. (2007). Pyoderma gangrenosum – a review. Orphanet Journal of Rare Diseases, 2(1), 19. doi:10.1186/1750-1172-2-19
4. Agathangelou C. (2009, Feb). Large necrotic malodorous pressure ulcer closed using unique silver dressings. Poster #35 presented at the 11th Biennial Conference of the NPUAP, Arlington VA. USA.
5. Benskin L. L. L. (2012). PolyMem Wic Silver Rope: A multifunctional dressing for decreasing pain, swelling, and inflammation. Advances in Wound Care. 1(1):44–7.
doi:10.1089/wound.2011.0285
6. Benskin LL. Polymeric Membrane Dressings for Topical Wound Management of Patients With Infected Wounds in a Challenging Environment: A Protocol With 3 Case Examples. Ostomy Wound Manage. 2016 Jun;62(6):42–50.
7. Benskin LL. Inflammation Relief Provides Key to Healing for Patient with Circumferential Pyoderma Gangrenosum [Internet]. 46th Annual Conference of the Wound, Ostomy, Continence Nurses Society; 2014 Jun 21; Nashville, TN. Available from: https://www.woundsource.com/poster/pain-relief-provides-key-healing-patient-circumferential-pyoderma-gangrenosum

.png)