Practice Innovations
(PI-001 (GR-010)) Preventing Foot Ulceration by Identification of Skin at Risk for Ulceration Utilizing Near Infrared Spectroscopy (NIRS) and Monitoring Off-Loading Utilizing NIRS
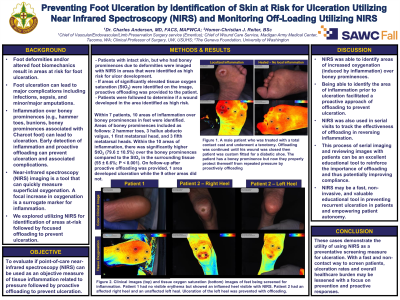
Foot deformities and/or altered foot biomechanics result in areas at risk for foot ulceration. Foot ulceration can lead to major complications including infections, sepsis and minor or major amputations. Inflammation over boney prominences, for example hammer toes, bunions or boney prominences associated with Charcot foot, can lead to ulceration. Early detection of inflammation and proactive offloading can prevent ulceration and associated complications. Near Infrared Spectroscopy (NIRS) imaging is a tool that can quickly measure superficial oxygenation. A focal increase in oxygenation is a surrogate marker for inflammation. We explored utilizing NIRS for identification of areas at-risk followed by focused offloading to prevent ulceration.
Methods: Patients with intact skin, but who had boney prominences due to deformities had the areas of interest imaged with NIRS. If these areas at risk for ulceration had increased tissue oxygen saturation (StO2) compared to surrounding tissue they were felt to be at risk for ulceration. These patients were then treated with proactive offloading. Patients were followed to determine if a wound developed in the area identified.
Results: Seven patients with 10 areas of inflammation over boney prominences in feet were identified. Areas of boney prominences included were: 2 hammer toes, 3 hallux adbucto valgus, 1 first metatarsal head and 3 fifth metatarsal heads. Within the 10 areas of inflammation, there was significantly higher StO2 (79.6% +/-10.5) over the boney prominences compared to the StO2 in the surrounding tissue (55% , +/-6.6; p< 0.001). On follow-up after proactive offloading was provided, 1 area developed an ulceration, 9 did not.
Discussion: NIRS was able to identify areas of increased oxygenation (inflammation) over boney prominences. Early areas of inflammation prior to ulceration facilitated a proactive approach of offloading to prevent ulceration. NIRS was also used in serial visits to track the effectiveness of offloading in reversing inflammation. Review of images with the patient can also be an excellent educational tool to reinforce the importance of offloading thus potentially improving compliance.
Trademarked Items:
References: References 1. Schaper, Van Netten, J. J., Apelqvist, J., Lipsky, B. A., & Bakker, K. (2016). Prevention and management of foot problems in diabetes: a Summary Guidance for Daily Practice 2015, based on the IWGDF Guidanc 1,2 2,3,4 2,5 2 2 2 1/13/23, 6:42 PM Preview - SAWC Spring 2023 Abstract SubmissionSubmissionID=1438352 3/3 e Documents. Diabetes/metabolism Research and Reviews, 32(S1), 7–15. https://doi.org/10.1002/dmrr.26 95 2. Tang, Zügner, R., Lisovskaja, V., Karlsson, J., Hagberg, K., & Tranberg, R. (2015). Foot deformities, funct ion in the lower extremities, and plantar pressure in patients with diabetes at high risk to develop foot ul cers. Diabetic Foot & Ankle, 6(1), 27593–27593. https://doi.org/10.3402/dfa.v6.27593 3. Malhotra, Bello, E., & Kominsky, S. (2012). Diabetic Foot Ulcerations: Biomechanics, Charcot Foot, an d Total Contact Cast. Seminars in Vascular Surgery, 25(2), 66–69. https://doi.org/10.1053/j.semvascsurg.2 012.05.001 4. Hedegaard Andersen, Rasmussen, A., Frimodt-Møller, M., Rossing, P., Kirketerp-Møller, K., & Engberg, S. (2019). The effect of needle tenotomy on hammer, mallet and claw toe deformities in patients with dia betes, a retrospective study. Journal of Clinical & Translational Endocrinology, 18, 100208–100208. http s://doi.org/10.1016/j.jcte.2019.100208 5. William J. Jeffcoate, Loretta Vileikyte, Edward J. Boyko, David G. Armstrong, Andrew J.M. Boulton; Curr ent Challenges and Opportunities in the Prevention and Management of Diabetic Foot Ulcers. Diabetes C are 1 April 2018; 41 (4): 645–652. https://doi.org/10.2337/dc17-1836

.png)
