Clinical Research
(CR-025) Outcomes of Mechanical Thrombectomy for the Treatment of Deep Vein Thrombosis-associated Venous Leg Ulcers
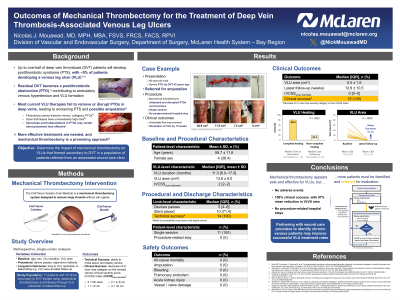
Methods: All patients with VLUs secondary to DVT referred to our center from August 2021 through May 2022 who were deemed candidates for MT with the study device* were retrospectively assessed. Technical success was crossing the PTO and deploying the MT catheter. Stents were placed in iliac segments if >50% vessel area reduction was observed by intravascular ultrasound. Using the revised venous clinical severity score (rVCSS), clinical success was a decrease of ≥1 ulcer diameter category (rVCSSdiameter; no VLU: 0, mild [< 2 cm]: 1, moderate [2–6 cm]: 2, severe [ >6 cm]: 3) at last follow-up.
*ClotTriever Thrombectomy System, Inari Medical, Irvine, California
Results:
Eleven patients with 15 VLUs on 14 limbs underwent MT (age: 59.7±11.8 years, women: 4 [36.4%]). Median VLU duration was 11.0 [interquartile range 6.0–17.0] months; 2 (18.2%) patients presented with VLUs persisting >40 years. Baseline VLU area was 13.6±9.0 cm2, and median rVCSSdiameter was 2 [2–2]. Technical success was achieved in all limbs. All limbs received adjunctive venoplasty, with stents placed in 10 (71.4%). No fibrinolytics were administered, and 0 adverse events occurred. No patient was admitted after thrombectomy due to the procedure. All VLUs demonstrated clinical success. The rVCSSdiameter improved to 0 [0–0] by last follow-up at 12.8±10.5 weeks. Twelve (80.0%) VLUs completely resolved by 10 [7–14] weeks. Three (20.0%) remaining VLUs demonstrated an 83.1±13.8% area reduction at 12 [6–12] weeks.
Discussion: All patients showed complete or near-complete VLU healing within months of a procedure that included MT. These preliminary results suggest that implementing MT with the study device in conjunction with adjuvant methods assists in reestablishing patency and cephalad flow, allowing VLUs to heal.
Trademarked Items: ClotTriever
References: 1. Dronkers CEA, Mol GC, Maraziti G, et al. Predicting Post-Thrombotic Syndrome with Ultrasonographic Follow-Up after Deep Vein Thrombosis: A Systematic Review and Meta-Analysis. Thromb Haemost. Aug 2018;118(8):1428-1438. doi:10.1055/s-0038-1666859.
2. Prandoni P, Lensing AW, Prins MH, et al. The impact of residual thrombosis on the long-term outcome of patients with deep venous thrombosis treated with conventional anticoagulation. Semin Thromb Hemost. Mar 2015;41(2):133-40. doi:10.1055/s-0035-1544161.
3. Ashrani AA, Heit JA. Incidence and cost burden of post-thrombotic syndrome. J Thromb Thrombolysis. Nov 2009;28(4):465-76. doi:10.1007/s11239-009-0309-3.
4. Yuriditsky E, Narula N, Jacobowitz GR, et al. Histological Assessment of Lower Extremity Deep Vein Thrombi from Patients Undergoing Percutaneous Mechanical Thrombectomy. J Vasc Surg Venous Lymphat Disord. 2021;S2213-333X(21):00176-1. doi:10.1016/j.jvsv.2021.03.010
5. Czaplicki C, Albadawi H, Partovi S, et al. Can thrombus age guide thrombolytic therapy? Cardiovasc Diagn Ther. Dec 2017;7(Suppl 3):S186-S196. doi:10.21037/cdt.2017.11.05.
6. Silver MJ, Kawakami R, Jolly MA, et al. Histopathologic analysis of extracted thrombi from deep venous thrombosis and pulmonary embolism: Mechanisms and timing. Catheter Cardiovasc Interv. Jun 1 2021;97(7):1422-1429. doi:10.1002/ccd.29500.
7. Schulman S, Lindmarker P, Holmstrom M, et al. Post-thrombotic syndrome, recurrence, and death 10 years after the first episode of venous thromboembolism treated with warfarin for 6 weeks or 6 months. J Thromb Haemost. 2006;4:734-42. doi:10.1111/j.1538-7836.2006.01795.x.
8. De Maeseneer MG, Kakkos SK, Aherne T, et al. Editor's Choice - European Society for Vascular Surgery (ESVS) 2022 Clinical Practice Guidelines on the Management of Chronic Venous Disease of the Lower Limbs. Eur J Vasc Endovasc Surg. Feb 2022;63(2):184-267. doi:10.1016/j.ejvs.2021.12.024.
9. Seager MJ, Busuttil A, Dharmarajah B, Davies AH. Editor's Choice-- A Systematic Review of Endovenous Stenting in Chronic Venous Disease Secondary to Iliac Vein Obstruction. Eur J Vasc Endovasc Surg. Jan 2016;51(1):100-20. doi:10.1016/j.ejvs.2015.09.002.
10. Dexter DJ, Kado H, Schor J, et al. Interim outcomes of mechanical thrombectomy for deep vein thrombosis from the All-Comer CLOUT Registry. J Vasc Surg Venous Lymphat Disord. Feb 24 2022;10(4):832-840.E2. doi:10.1016/j.jvsv.2022.02.013.
11. Maldonado TS, Dexter DJ, Kado H, et al. Outcomes from the ClotTriever Outcomes Registry show symptom duration may underestimate deep vein thrombus chronicity. J Vasc Surg Venous Lymphat Disord. 2022;10(6):1251-1259. doi:10.1016/j.jvsv.2022.04.015.
12. Mouawad NJ. Chronic Venous Ulcer Resolution and Post-Thrombotic Syndrome Improvement After Percutaneous Mechanical Thrombectomy of a Forty-Two-Year-Old DVT. Journal of Vascular Surgery Cases, Innovations and Techniques. 2022;doi:10.1016/j.jvscit.2022.03.001.

.png)
