Case Series/Study
(CS-102) Limb Salvage in a Complex Patient Undergoing Multiple Lower Extremity Amputations with Placental Extracellular Matrix (PECM)
Patients with diabetes mellitus type II (DMII) and peripheral arterial disease (PAD) can develop wounds that are difficult to treat due to lack of blood flow and nutrients to the lower extremity. Even after revascularization, the already challenging situation of being diabetic with a wound can still lead to complications, including high-level amputations.1 The goal of this case study is to demonstrate the use of PECM* to facilitate the development of granulation tissue in the treatment of a complex patient and salvage the lower limb.
Methods:
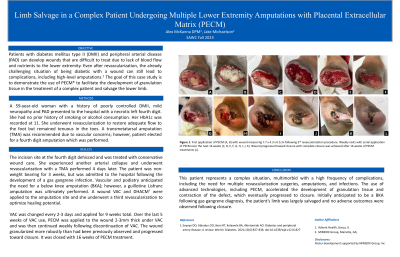
A 59-year-old woman with a history of poorly controlled DMII, mild neuropathy and PAD presented to the hospital with a necrotic left fourth digit. She had no prior history of smoking or alcohol consumption. Her HbA1c was recorded at 11. She underwent revascularization to restore adequate flow to the foot but remained tenuous in the toes. A transmetatarsal amputation (TMA) was recommended due to vascular concerns; however, patient elected for a fourth digit amputation which was performed.
Results:
The incision site at the fourth digit dehisced and was treated with conservative wound care. She experienced another arterial collapse and underwent revascularization with a TMA performed 4 days later. The patient was non-weight bearing for 3 weeks, but was admitted to the hospital following the development of a gas gangrene infection. Vascular and podiatry anticipated the need for a below knee amputation (BKA); however, a guillotine Lisfranc amputation was ultimately performed. A wound VAC and DHACM** were applied to the amputation site and she underwent a third revascularization to optimize healing potential.
VAC was changed every 2-3 days and applied for 9 weeks total. Over the last 5 weeks of VAC use, PECM was applied to the wound 2-3mm thick under VAC and was then continued weekly following discontinuation of VAC. The wound granularized more robustly than had been previously observed and progressed toward closure. It was closed with 16 weeks of PECM treatment.
Discussion:
This patient represents a complex situation, multimorbid with a high frequency of complications, including the need for multiple revasculariztion surgeries, amputations, and infections. The use of advanced technologies, including PECM, accelerated the development of granulation tissue and contraction of the defect, which eventually progressed to closure. Initially anticipated to be a BKA following gas gangrene diagnosis, the patient’s limb was largely salvaged and no adverse outcomes were observed following closure.
Trademarked Items:
References: 1. Soyoye DO, Abiodun OO, Ikem RT, Kolawole BA, Akintomide AO. Diabetes and peripheral artery disease: A review. World J Diabetes. 2021;12(6):827-838. doi:10.4239/wjd.v12.i6.827

.png)