Case Series/Study
(CS-093) Large Refractory Atypical Buttock Wound From Systemic Fungal Infection Heals with Novel Transforming Powder Dressing: Case Study of a Critically Ill Nine-Year-Old Male
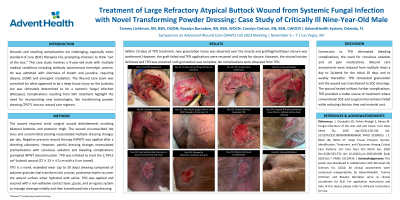
Wounds and resulting complications are challenging, especially when standard of care (SOC) therapies fail, prompting clinicians to think “out of the box.” This case study involves a 9-year-old male with multiple medical conditions including antibody autoimmune hemolytic anemia who was admitted with shortness of breath and jaundice, resulting in complicated hospital course requiring dialysis, ECMO and emergent intubation. The Wound Care team was consulted for what appeared to be a deep tissue injury on the buttocks, but was ultimately determined to be a systemic fungal infection (Rhizopus). This case highlights the need for incorporating new technologies, like transforming powder dressing (TPD) into our wound care regimes.
Methods:
The patient’s wound required serial surgical wound debridement involving bilateral buttocks and posterior thigh. The wound circumscribed the anus and uncontrolled stooling necessitated multiple daily dressing changes. Negative pressure wound therapy (NPWT) was not applied until a diverting colostomy was created. NPWT dressings required premedication with conscious sedation for pain management. Bleeding complications prompted NPWT discontinuation, and TPD was initiated to treat the 2,794.5 cm3 buttock wound (27 x 23 x 4.5 cm with a 6 cm tunnel).
TPD is a novel, extended wear (up to 30 days) dressing comprised of polymers similar to those used in contact lenses. It transforms into a moist, protective matrix that covers the wound surface when hydrated with saline. TPD was initially applied 3x/week along with a non-adhesive contact layer, gauze, and an egress system to manage drainage.
Results:
Within 10 days, new granulation tissue was observed over the muscle and grafting/multilayer closure was performed, however, the graft failed. Weekly TPD applications were resumed until re-epithelialization (11 months). No complications were observed from TPD.
Discussion:
Conversion to TPD eliminated bleeding complications, the need for conscious sedation and all pain medications. Wound care assessments were reduced from daily to 2x/week, resulting in reduced clinician time and material costs, without further complications. TPD provided a viable alternative in this patient where conventional SOC failed.
Trademarked Items:
References:

.png)