Case Series/Study
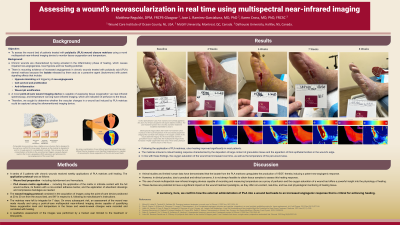
(CS-123) Assessing a wound’s neovascularization in real time using multispectral near-infrared imaging
Jose Ramirez-Garcialuna, MD, PhD
Introduction:
Methods:
Results:
Discussion:
Trademarked Items: MIMOSA, SupraSDRM
References: Mirhaj M, Labbaf S, Tavakoli M, Seifalian AM. Emerging treatment strategies in wound care. Int Wound J. 2022 Nov;19(7):1934–54.
Ring A, Goertz O, Al-Benna S, Ottomann C, Langer S, Steinstraesser L, et al. Accelerated angiogenic induction and vascular integration in a novel synthetic scaffolding matrix for tissue replacement. Int J Artif Organs. 2010 Dec;33(12):877–84.
Haller HL, Sander F, Popp D, Rapp M, Hartmann B, Demircan M, et al. Oxygen, pH, Lactate, and Metabolism—How Old Knowledge and New Insights Might Be Combined for New Wound Treatment. Medicina. 2021 Nov;57(11):1190.
Ramirez-GarciaLuna JL, Bartlett R, Arriaga-Caballero JE, Fraser RDJ, Saiko G. Infrared Thermography in Wound Care, Surgery, and Sports Medicine: A Review. Front Physiol. 2022;13:838528.
Saiko G, Lombardi P, Au Y, Queen D, Armstrong D, Harding K. Hyperspectral imaging in wound care: A systematic review. Int Wound J. 2020 Dec;17(6):1840–56.
Chronic wounds are characterized by impaired neo-angiogenesis, which causes local hypoxia and lowers the healing potential. Pre-clinical data has shown increased angiogenesis of wounds treated with polylactic acid (PLA) matrices. Therefore, the objective of this research was to assess the bed of wounds treated with PLA matrices using a novel optical device to quantify tissue oxygenation levels.
Methods:
A series of 5 patients with chronic wounds received weekly applications of PLA matrices until healing. The matrices were applied in direct contact with the wound bed, surgically fixed, and left to integrate for 7 days. On the next visit, an assessment of the wound was made visually and using a point-of-care multispectral near-infrared imaging device capable of quantifying tissue oxygenation level and temperature in the tissue. Week-to-week changes were recorded and correlated with wound healing.
Results:
Following the application of PLA matrices, ulcer healing improved significantly in most patients. The matrices induced a robust healing response characterized by the deposition of large content of granulation tissue and the apparition of thick epithelial borders in the wound’s edge. In line with these findings, the oxygen saturation of the wound bed increased over time, as well as the temperature of the peri-wound area.
Discussion:
The lactate present in PLA matrices upregulates the production of VEGF and induces a potent neo-angiogenic response. Preclinical data have demonstrated this effect, however, for practical and ethical concerns, it is not always feasible to obtain tissue biopsies to assess the healing response in wounds. The use of novel multispectral near-infrared imaging devices capable of quantifying temperature as a proxy measure of perfusion and the oxygen saturation of a wound bed offers a powerful insight into the physiology of healing. Here, we confirm how the external administration of lactate into a wound bed leads to an increased angiogenic response that is critical for achieving healing.
Trademarked Items: MIMOSA, SupraSDRM
References: Mirhaj M, Labbaf S, Tavakoli M, Seifalian AM. Emerging treatment strategies in wound care. Int Wound J. 2022 Nov;19(7):1934–54.
Ring A, Goertz O, Al-Benna S, Ottomann C, Langer S, Steinstraesser L, et al. Accelerated angiogenic induction and vascular integration in a novel synthetic scaffolding matrix for tissue replacement. Int J Artif Organs. 2010 Dec;33(12):877–84.
Haller HL, Sander F, Popp D, Rapp M, Hartmann B, Demircan M, et al. Oxygen, pH, Lactate, and Metabolism—How Old Knowledge and New Insights Might Be Combined for New Wound Treatment. Medicina. 2021 Nov;57(11):1190.
Ramirez-GarciaLuna JL, Bartlett R, Arriaga-Caballero JE, Fraser RDJ, Saiko G. Infrared Thermography in Wound Care, Surgery, and Sports Medicine: A Review. Front Physiol. 2022;13:838528.
Saiko G, Lombardi P, Au Y, Queen D, Armstrong D, Harding K. Hyperspectral imaging in wound care: A systematic review. Int Wound J. 2020 Dec;17(6):1840–56.

.png)