Case Series/Study
(CS-108) First Reported Use of Lyophilized Human Amnion Chorion Membrane (LHACM*) in the Treatment of a Diabetic Foot Ulcer in a Charcot Patient
Five-year mortality risk for patients with Charcot foot rival the pooled all cancers risk and outnumber the breast cancer five-year risk of mortality.1 Diabetic foot ulcers (DFUs) affect 19% to 34% of patients with diabetes and continue to challenge clinicians.2 Per CMS3 and CAMPs4 guidelines, after four weeks of standard of care (SOC), with less than 50% surface area reduction, wounds, including DFUs, are considered chronic. Current recommended guidelines suggest that advanced therapies, including placental-based allografts, be considered for chronic wounds.3,4 LHACM, a new, novel tri-layer placental-based allograft intended for deeper and complex wounds, is presented in this case study.
Methods:
A 64-year-old male was referred for evaluation of a chronic Grade III Wagner DFU three months after onset. The patient’s healthcare history includes DM with neuropathy, Charcot with reconstruction, hypertension, hypercholesterolemia, asthma, and a previous DFU on the affected foot. He is independent, lives alone, and denies smoking or alcohol use.
Results:
SOC, which included weekly sharp curette debridement, a multitude of dressings and advanced care therapies, 30-40 mmHg compression wrap, and an offloading insole shoe† was employed for 15 weeks without resolution. Advanced therapies included other allografts and dressings included alginate wound dressing and collagen dressing‡ with alginate wound dressing.
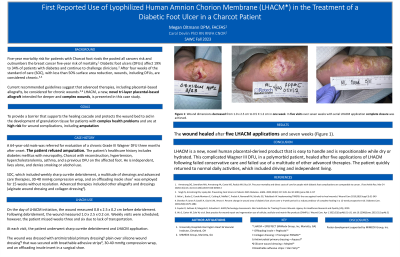
On the day of LHACM initiation, prior to debridement, the wound measured 0.8 x 2.5 x 0.2 cm. Following debridement, the wound measured 1.0 x 2.5 x 0.2 cm. Weekly visits were scheduled; however, the patient missed weeks three and six due to lack of transportation. At each visit, the patient underwent sharp curette debridement and LHACM application. Post debridement measurement at week 6 was reduced to 0.5 x 1.2 x 0.1 cm. The wound was dressed with antimicrobial primary dressing§ plain over silicone wound dressing¶ that was secured with breathable adhesive strips#, 30-40 mmHg compression wrap, and an offloading insole insert in a surgical shoe. After five LHACM applications and seven weeks the wound healed.
Discussion:
LHACM is a new, novel placental derived product that is easy to handle and is repositionable while dry or hydrated. This complicated Wagner III DFU, in a polymorbid patient, healed after five application of LHACM following failed conservative care and failed use of a multitude of other advanced therapies. The patient quickly returned to normal daily activities, which included driving and independent living.
Trademarked Items: *LHACM = EPIEFFECT (MiMedx Group, Inc, Marietta, GA)
† Offloading insole = PegAssist™
‡ Collagen dressing = Promogran PRISMA™
§ Antimicrobial primary dressing = Aquacel®
¶ Silicone wound dressing = Mepitel®
# Breathable adhesive strips = Steri Strip™
References: 1. Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, Bus SA. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res. Mar 24 2020;13(1):16. doi:10.1186/s13047-020-00383-2
2. Singh N, Armstrong DG, Lipsky BA. Preventing Foot Ulcers in Patients With Diabetes. JAMA. 2005;293(2):217-228. doi:10.1001/jama.293.2.217
3. Snyder D, Sullivan N, Margolis D, Schoelles K. AHRQ Technology Assessments. Skin Substitutes for Treating Chronic Wounds. Agency for Healthcare Research and Quality (US); 2020.
4. Wu S, Carter M, Cole W, et al. Best practice for wound repair and regeneration use of cellular, acellular and matrix-like products (CAMPs). J Wound Care. Apr 1 2023;32(Sup4b):S1-s31. doi:10.12968/jowc.2023.32.Sup4b.S1

.png)