Practice Innovations
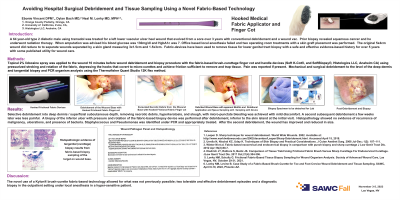
(PI-025) Avoiding Hospital Surgical Debridement and Tissue Sampling Using a Novel Fabric-Based Technology
A 64 year-old type 2 diabetic male using tramadol was treated for a left lower vascular ulcer heel wound that evolved from a sore over 3 years with conventional debridement and a wound vac. Prior biopsy revealed squamous cancer and he underwent radiation therapy. When amputation was advised his blood glucose was 130mg/dl and HgbA1c was 7. Office based local anesthesia failed and two operating room treatments with a skin graft placement was performed. The original 5x4cm wound did reduce to to separate wounds separated by a skin gland measuring 3x1.5cm and 1.5x3cm. Fabric-devices have been used to remove tissue for lower genital tract biopsy with a safe and effective evidence-based history for over 5 years with some published utility for wound care.
Methods:
Topical 2% lidocaine spray was applied to the wound 10 minutes before wound debridement and biopsy procedure with the fabric-based brush-curettage finger cot and handle devices (Soft K-Cot®, and SoftBiopsy®) using pressurized stroking and rotation of the fabric, depressing the hooks that covert to micro-curettes and achieve friction sufficient to remove and trap tissue. Pain was reported if present. Mechanical and surgical debridement to the level of the deep dermis and tangential biopsy and PCR organism analysis using the Thermofisher Quant Studio 12K flex method.
Results:
Selective debridement into deep dermis removing necrotic debris, hyperkeratosis, and slough, with micro-punctate bleeding was achieved with mild discomfort. A second subsequent debridement a few weeks later was less painful. A biopsy of the inferior ulcer with pressure and rotation of the fabric-based biopsy device was performed after debridement, inferior to the skin island at the initial visit. Histopathology showed no evidence of recurrence of malignancy, ulcerations, and presence of bacteria. Staphylococcus and Pseudomonas was identified under PCR and appropriately treated. After the second debridement, the wound has improved and reduced in size.
Discussion: The novel use of a Kylon® brush-curette fabric-based technology allowed for what was not previously possible; two tolerable and effective debridement episodes and a diagnostic biopsy in the outpatient setting under local anesthesia in a hyper-sensitive patient.
Trademarked Items: Kylon® medical fabric, Soft K-Cot®, SoftBiopsy®
References: References
1. Leaper D. Sharp technique for wound debridement. World Wide Wounds. 2002. Available at: https://www.worldwidewounds.com/2002/december/Leaper/Sharp-Debridement.html. Accessed April 15, 2018.
2. Urmila N, Nischal KC, Uday K. Techniques of Skin Biopsy and Practical Considerations. J Cutan Aesthet Surg. 2008 Jul-Dec; 1(2): 107–111.
3. Winter M et al. Fabric-based exocervical and endocervical biopsy in comparison with punch biopsy and sharp curettage J Low Genit Tract Dis. 2012 Apr;16(2):80-7.
4. Diedrich JT, Rathore S, Bentz JS. Comparison of Tissue Yield Using Frictional Fabric Brush Versus Sharp Curettage For Endocervical Curettage. J Low Genit Tract Dis. 2017 Oct;21(4):304-306.
5. Lonky NM, Schultz G. Frictional Fabric-Based Tissue Biopsy Sampling for Wound Organism Analysis. Society of Advanced Wound Care, Las Vegas, NV, October 29-31, 2021.
6. Lonky NM, Levine B. Case Study of a Fabric-Based Brush-Curette for Toe and Foot Crevice Wound Debridement and Tissue Sampling. SAWC, April 8-10, 2022, Phoenix AZ.

.png)