Case Series/Study
(CS-128) 1% TBSA Superficial Partial Thickness Wound Complicated by Peripheral Vascular Disease & Diabetes Mellitus
Emilee Hart, PT, DPT
Introduction: Patients who develop burns and have underlying diabetes mellitus (DM) are at increased risk for poor outcomes. Patients with DM can have pre-existing complications including peripheral neuropathy, peripheral vascular disease, and retinopathy. These complications arise with uncontrolled diabetes and place patients at an increased risk for non-healing wounds, amputations, and mortality as a result of their altered physiology.
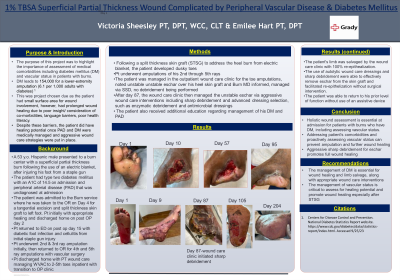
Methods: A 53 y.o. Hispanic male presented to a burn center with a superficial partial thickness burn following the use of an electric blanket, after injuring his foot from a staple gun. The patient had type two diabetes mellitus with an A1C of 14.5 on admission and peripheral arterial disease (PAD) that was undiagnosed at admission. Following a split thickness skin graft (STSG) to address the heel burn, the patient developed dusky toes, and eventually underwent amputations of his 2nd through 5th rays. The patient was managed in the outpatient wound care clinic for the toe amputations and developed unstable eschar over his heel skin graft that was not managed by the burn clinic. The wound care clinic utilized aggressive wound care interventions, including sharp debridement and advanced dressing selection. The patient also received additional education regarding management of his DM.
Results: The patient's limb was ultimately able to be salvaged by the wound care clinic. The use of autolytic wound care dressings and sharp debridement were able to effectively remove eschar from the skin graft and facilitated re-epithelization. The patient was able to return to his prior level of function and achieved 100% wound re-epithelization.
Discussion: This case highlights the importance of holistic wound assessment at admission for patients with burns who have DM, including assessing vascular status. Education regarding management of DM is essential for wound healing and limb salvage, along with appropriate wound care interventions.
Trademarked Items:
References:
Methods: A 53 y.o. Hispanic male presented to a burn center with a superficial partial thickness burn following the use of an electric blanket, after injuring his foot from a staple gun. The patient had type two diabetes mellitus with an A1C of 14.5 on admission and peripheral arterial disease (PAD) that was undiagnosed at admission. Following a split thickness skin graft (STSG) to address the heel burn, the patient developed dusky toes, and eventually underwent amputations of his 2nd through 5th rays. The patient was managed in the outpatient wound care clinic for the toe amputations and developed unstable eschar over his heel skin graft that was not managed by the burn clinic. The wound care clinic utilized aggressive wound care interventions, including sharp debridement and advanced dressing selection. The patient also received additional education regarding management of his DM.
Results: The patient's limb was ultimately able to be salvaged by the wound care clinic. The use of autolytic wound care dressings and sharp debridement were able to effectively remove eschar from the skin graft and facilitated re-epithelization. The patient was able to return to his prior level of function and achieved 100% wound re-epithelization.
Discussion: This case highlights the importance of holistic wound assessment at admission for patients with burns who have DM, including assessing vascular status. Education regarding management of DM is essential for wound healing and limb salvage, along with appropriate wound care interventions.
Trademarked Items:
References:

.png)