Case Series/Study
(CS-096) A Novel approach to eliminating Pseudomonas biofilm in a chronic wound using non-contact, low-frequency ultrasound therapy with saline mist
Michael Jensen, MD, CWSP – Chief Medical Officer, Kane Wound Care; Kavita Talati, APN, CWS – Wound Nurse Practitioner
Introduction: Evidence shows healing times for both acute and chronic wound are negatively affected by the presence of biofilm (Gajula et al., 2020). The occurrence of biofilm in chronic wounds is estimated to be 78.2% (Malone et al., 2017). Pseudomonas aeruginosa is a common microbe present in wound biofilm. Traditionally, sharp debridement in conjunction with topical antimicrobial therapy has been the mainstay method for reducing levels of Pseudomonas aeruginosa in a wound. More recently, noncontact, low-frequency ultrasound treatment delivered through a saline mist is being recognized as an effective approach to removing biofilm and can be more beneficial than sharp debridement (Dhar & Han, 2020). The goal of this case study is to explore the effects of ultrasound therapy with saline mist on Pseudomonas aeruginosa colonization as evidenced by autofluorescence imaging.
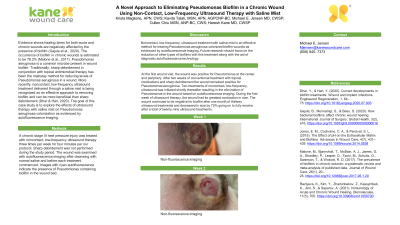
Methods: A chronic stage III heel pressure injury was treated with noncontact, low-frequency ultrasound therapy three times per week for four minutes per our protocol. Sharp debridement was not performed during the study period. The wound was examined with autofluorescence imaging after cleansing with normal saline and before each treatment commenced. Images with cyan autofluorescence indicate the presence of Pseudomonas containing biofilm in the wound bed.
Results: At the first wound visit, the wound was positive for Pseudomonas at the center and periphery. After two weeks of conventional treatment with topical medications and sharp debridement the wound remained positive for Pseudomonas aeruginosa. Two treatments of noncontact, low-frequency, ultrasound was initiated shortly thereafter resulting in the elimination of Pseudomonas in the wound based on autofluorescence imaging. During the first week of ultrasound therapy, the wound had its greatest contraction in size. The wound continued to be negative for biofilm after one month of thirteen ultrasound treatments and decreased in size by 75% going on to fully resolve after a total of twenty-nine ultrasound treatments.
Discussion: Noncontact, low-frequency, ultrasound treatment with saline mist is an effective method for treating Pseudomonas aeruginosa-colonized biofilm wounds as evidenced by autofluorescence imaging. Future research should focus on the reduction of other types of biofilms with this treatment along with the aid of diagnostic autofluorescence technology.
Trademarked Items:
References: Dhar, Y., & Han, Y. (2020). Current developments in biofilm treatments: Wound and implant infections. Engineered Regeneration, 1, 64–75. https://doi.org/10.1016/j.engreg.2020.07.003
Gajula, B., Munnamgi, S., & Basu, S. (2020). How bacterial biofilms affect chronic wound healing. International Journal of Surgery: Global Health, 3(2), e16. https://doi.org/10.1097/gh9.0000000000000016
Jones, E. M., Cochrane, C. A., & Percival, S. L. (2015). The Effect of pH on the Extracellular Matrix and Biofilms. Advances in Wound Care, 4(7), 431–439. https://doi.org/10.1089/wound.2014.0538
Malone, M., Bjarnsholt, T., McBain, A. J., James, G. A., Stoodley, P., Leaper, D., Tachi, M., Schultz, G., Swanson, T., & Wolcott, R. D. (2017). The prevalence of biofilms in chronic wounds: a systematic review and meta-analysis of published data. Journal of Wound Care, 26(1), 20–25. https://doi.org/10.12968/jowc.2017.26.1.20
Raziyeva, K., Kim, Y., Zharkinbekov, Z., Kassymbek, K., Jimi, S., & Saparov, A. (2021). Immunology of Acute and Chronic Wound Healing. Biomolecules, 11(5), 700. https://doi.org/10.3390/biom11050700
Methods: A chronic stage III heel pressure injury was treated with noncontact, low-frequency ultrasound therapy three times per week for four minutes per our protocol. Sharp debridement was not performed during the study period. The wound was examined with autofluorescence imaging after cleansing with normal saline and before each treatment commenced. Images with cyan autofluorescence indicate the presence of Pseudomonas containing biofilm in the wound bed.
Results: At the first wound visit, the wound was positive for Pseudomonas at the center and periphery. After two weeks of conventional treatment with topical medications and sharp debridement the wound remained positive for Pseudomonas aeruginosa. Two treatments of noncontact, low-frequency, ultrasound was initiated shortly thereafter resulting in the elimination of Pseudomonas in the wound based on autofluorescence imaging. During the first week of ultrasound therapy, the wound had its greatest contraction in size. The wound continued to be negative for biofilm after one month of thirteen ultrasound treatments and decreased in size by 75% going on to fully resolve after a total of twenty-nine ultrasound treatments.
Discussion: Noncontact, low-frequency, ultrasound treatment with saline mist is an effective method for treating Pseudomonas aeruginosa-colonized biofilm wounds as evidenced by autofluorescence imaging. Future research should focus on the reduction of other types of biofilms with this treatment along with the aid of diagnostic autofluorescence technology.
Trademarked Items:
References: Dhar, Y., & Han, Y. (2020). Current developments in biofilm treatments: Wound and implant infections. Engineered Regeneration, 1, 64–75. https://doi.org/10.1016/j.engreg.2020.07.003
Gajula, B., Munnamgi, S., & Basu, S. (2020). How bacterial biofilms affect chronic wound healing. International Journal of Surgery: Global Health, 3(2), e16. https://doi.org/10.1097/gh9.0000000000000016
Jones, E. M., Cochrane, C. A., & Percival, S. L. (2015). The Effect of pH on the Extracellular Matrix and Biofilms. Advances in Wound Care, 4(7), 431–439. https://doi.org/10.1089/wound.2014.0538
Malone, M., Bjarnsholt, T., McBain, A. J., James, G. A., Stoodley, P., Leaper, D., Tachi, M., Schultz, G., Swanson, T., & Wolcott, R. D. (2017). The prevalence of biofilms in chronic wounds: a systematic review and meta-analysis of published data. Journal of Wound Care, 26(1), 20–25. https://doi.org/10.12968/jowc.2017.26.1.20
Raziyeva, K., Kim, Y., Zharkinbekov, Z., Kassymbek, K., Jimi, S., & Saparov, A. (2021). Immunology of Acute and Chronic Wound Healing. Biomolecules, 11(5), 700. https://doi.org/10.3390/biom11050700

.png)