Case Series/Study
(CS-157) 12 Month Retrospective Review of Hidradenitis Suppurativa Plastic Surgical Excision and Reconstruction Techniques involving the use of pure Hypochlorous Acid (pHA) Preserved Wound Solution for Wound Bed Preparation.
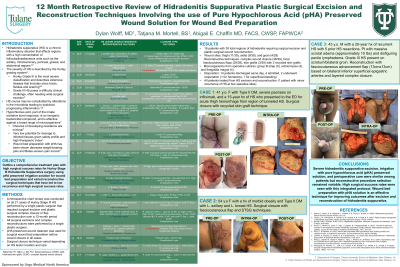
Severe hidradenitis suppurativa patients who present with chronic, fibrotic, and tunneled disease represent a difficult clinical challenge. These hidradenitis wounds are often refractory to dermatologic management and have underlying heavy microbial colonization. Surgical excision of the hidradenitis with plastic surgical reconstructive procedures may represent the only curative option. However, the rate of recurrence and complications after surgery remains high. We share our experience with a comprehensive treatment plan including operative resection, wound preparation with pure hypochlorous acid (pHA) preserved solution, and varied reconstructive surgical techniques, which have led to low recurrence and high surgical success rates.
Methods: Data was collected by retrospective review of all patients with Hurley Stage 3 hidradenitis suppurativa treated with surgical excision and various plastic surgical complex closure, skin graft, and flap techniques at one academic hospital from January 17, 2022 to January 17, 2023. 18 patients were recognized by these criteria with 21 operative episodes. Operative techniques and perioperative protocols were examined. In addition, patients’ demographics, comorbidities, and operative cultures were reviewed. Outcomes were assessed at discharge from postoperative care in the outpatient wound center based on presence of any recurrent hidradenitis and healing outcomes of the surgical sites
Results: 18 patients with 39 total regions of hidradenitis requiring surgical excision and plastic surgical wound closure were examined. The most common wound sites included thigh (11 of 39), axilla (9 of 39), and groin (4 of 39.) Dilute hypochlorous acid preserved solution irrigation was used before wound closure in all cases The most common reconstructive techniques were complex layered closure (36 of 39) combined with local fasciocutaneous flaps (29 of 39.) Skin grafts were used in 3 of 39 cases including 2 with recycled skin grafts. 14 patients were discharged same day and 4 were admitted. 2 patients underwent reoperation, one for hematoma and one for superficial bleeding. All patients healed from their hidradenitis excision and reconstruction with one patient with recurrence of HS at two operative sites. 6 patients were on immunomodulatory agents. The most common microorganisms grown were group B strep (5), actinomyces (4), and finegoldium magna (4.)
Discussion:
Severe hidradenitis suppurative excision, irrigation with pure hypochlorous acid (pHA) preserved solution irrigation, and perioperative care were similar among patients, but reconstructive procedure selection remained variable. High surgical success rates were seen with this integrated protocol. Wound bed preparation with pHA is an effective technique for improving outcomes after excision of hidradenitis suppurativa.
Trademarked Items:
References:

.png)